Dear Editors,
Kidney transplantation is one of the primary modalities of kidney replacement therapy (KRT) for patients with kidney failure. Compared with dialysis, it offers multiple advantages, including improved survival, better quality of life, and reduced healthcare costs [1, 2]. Therefore, understanding the implementation of kidney transplantation is essential for appropriate healthcare resource allocation and policy planning in each region. In Western countries, kidney transplantation is highly prevalent, with approximately 30%–50% of patients receiving KRT being transplant recipients [3, 4]. In contrast, in Japan, kidney transplantation remains a relatively limited treatment modality, primarily due to donor shortages and potential cultural factors [5–7].
The Japan Society for Transplantation, in collaboration with the Japanese Society for Clinical Renal Transplantation, has long collected detailed data at the time of transplantation, providing accurate statistics on the number of transplants and donor types [5–7]. However, long-term post-transplant follow-up is not always complete, leaving the number of kidney transplant recipients with functioning grafts (i.e., prevalent recipients) uncertain. This lack of information represents a significant limitation for evaluating the proportion of transplant recipients relative to patients on dialysis and for conducting international comparisons.
To address this, we estimated temporal trends in the number of prevalent kidney transplant recipients in Japan using summary statistics published by the Japan Society for Transplantation [5–7]. Furthermore, using data from the Japan Society for Dialysis Therapy Renal Data Registry [8], we calculated the proportion of prevalent kidney transplant recipients among all patients receiving KRT.
The annual numbers of living- and deceased-donor kidney transplants performed from 1964 to 2023, obtained from the Japan Society for Transplantation records [5–7], are summarized in Supplementary Figure S1 and Supplementary Table S1. The number of transplants was very low in the 1960s, gradually increased from the late 1970s, and has stabilized at approximately 1,500–2,000 per year since the 2010s. By 2023, a total of 47,466 transplants had been performed, comprising 39,543 living-donor and 7,923 deceased-donor transplants.
Temporal trends in the number of prevalent kidney transplant recipients, estimated based on graft survival for each era (Supplementary Figure S2), are shown in Figure 1a and Supplementary Table S2. The estimated number of prevalent recipients increased over time, reaching 27,935 living-donor recipients, 3,617 deceased-donor recipients, and a total of 31,552 recipients by 2023.
FIGURE 1
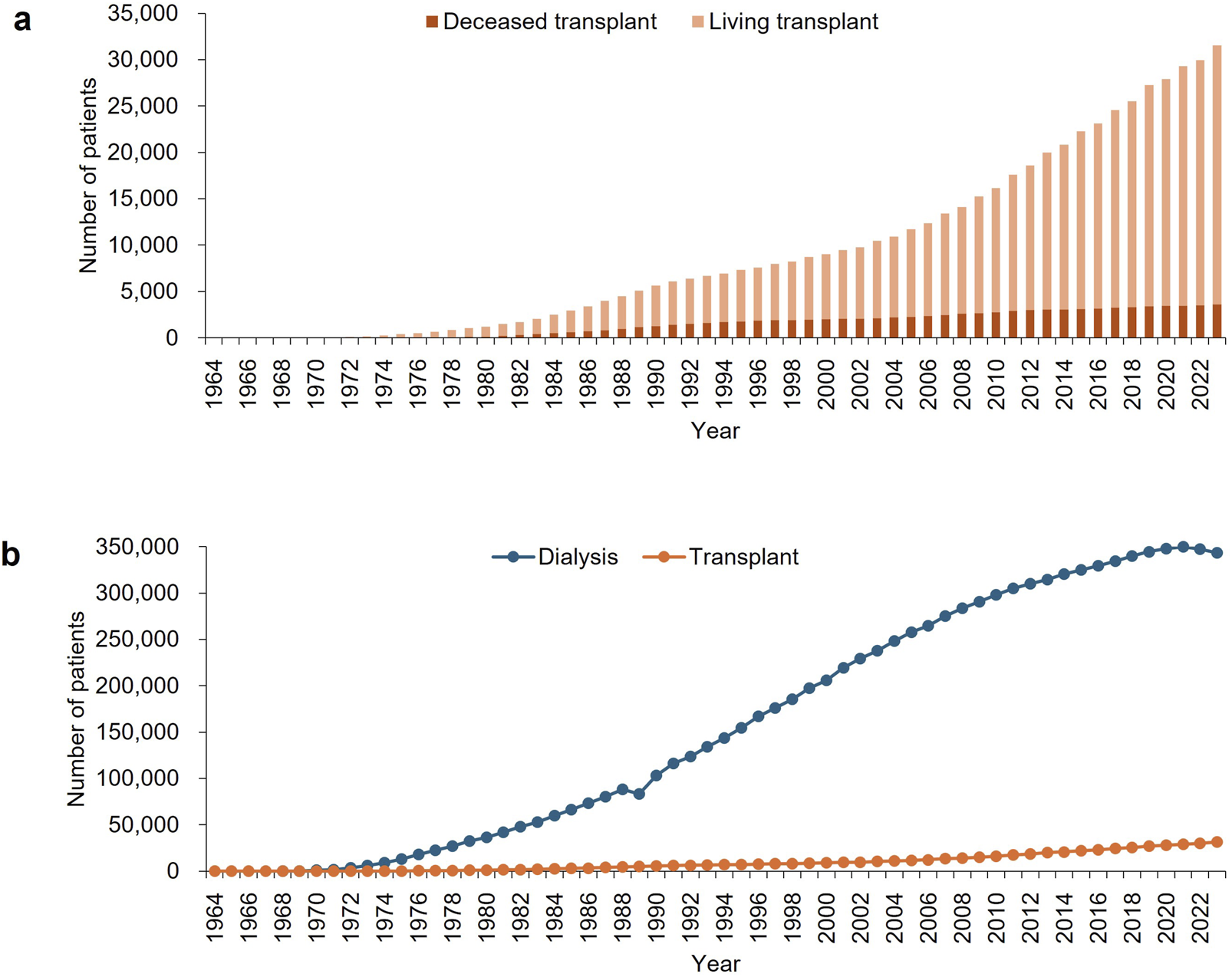
Temporal trends from 1964 to 2023 in (a) the estimated numbers of living- and deceased-donor prevalent kidney transplant recipients, and (b) the estimated total number of prevalent kidney transplant recipients, compared with the number of patients undergoing dialysis. Data on patients undergoing dialysis were obtained from the Japan Society for Dialysis Therapy Renal Data Registry [8]. Detailed numerical data are provided in Supplementary Tables S2, S3.
Temporal trends in the estimated number of prevalent kidney transplant recipients, compared with the number of patients on dialysis reported by the JSDT Renal Data Registry [8], are shown in Figure 1b and Supplementary Table S3. The proportion of these patients relative to the total population in Japan is shown in Supplementary Figure S3. The estimated proportion of prevalent kidney transplant recipients among all patients receiving KRT in Japan gradually increased over time, reaching 8.4% in 2023.
This study reports that the estimated number of prevalent kidney transplant recipients in Japan has steadily increased, surpassing 30,000 in 2023 and accounting for 8.4% of all patients receiving KRT. These data provide an important reference not only for understanding the current status of kidney transplantation in Japan, but also for enabling international comparisons and contributing to global discussions on transplantation practices.
A notable finding is that, compared with Western countries [3, 4], the proportion of prevalent kidney transplant recipients in Japan remains low, primarily due to the limited number of deceased-donor transplants. Contributing factors include delayed societal recognition of brain-dead organ donation, regulatory constraints, and challenges in obtaining family consent [9]. In addition, population aging and advances in chronic kidney disease management have led to an older demographic among patients requiring KRT [8], which may limit eligibility for kidney transplantation. Nonetheless, we observed a steady increase in prevalent recipients, likely reflecting both the gradual increase in the number of kidney transplants and the favorable long-term outcomes of kidney transplantation in Japan [5–7].
This study has several limitations. Most importantly, the estimates were derived from registry-reported transplant numbers and graft survival rates, rather than from a direct count of prevalent recipients. The graft survival rates were based on recipients with available follow-up, so outcomes of those lost to follow-up may differ. Furthermore, this secondary analysis relied entirely on summary data without access to individual-level information. Further investigation is needed to collect comprehensive patient-level data on prevalent kidney transplant recipients. The newly developed national transplant registry system, TRACER (TRAnsplant CEntral Registry), may help address these gaps.
In conclusion, kidney transplantation remains a relatively uncommon KRT modality in Japan, but the number of recipients with functioning grafts has steadily increased. Continued efforts are needed to refine these estimates and to establish a robust foundation for meaningful international comparisons.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
HK conducted the analysis and drafted the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declared that financial support was not received for this work and/or its publication.
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontierspartnerships.org/articles/10.3389/ti.2025.15732/full#supplementary-material
References
1.
Tonelli M Wiebe N Knoll G Bello A Browne S Jadhav D et al Systematic Review: Kidney Transplantation Compared with Dialysis in Clinically Relevant Outcomes. Am J Transpl (2011) 11(10):2093–109. 10.1111/j.1600-6143.2011.03686.x
2.
Laupacis A Keown P Pus N Krueger H Ferguson B Wong C et al A Study of the Quality of Life and Cost-Utility of Renal Transplantation. Kidney Int (1996) 50(1):235–42. 10.1038/ki.1996.307
3.
Boenink R Bonthuis M Boerstra BA Astley ME Montez de Sousa IR Helve J et al The ERA Registry Annual Report 2022: Epidemiology of Kidney Replacement Therapy in Europe, with a Focus on Sex Comparisons. Clin Kidney J (2025) 18(2):sfae405. 10.1093/ckj/sfae405
4.
United States Renal Data System. 2024 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (2024). Available online at: https://usrds-adr.niddk.nih.gov/2024 (Accessed October 5, 2025).
5.
Sonoda T Shikata M Miyamoto H . Proceedings of the 3rd Clinical Meeting on Kidney Transplantation. Jpn J Transpl (1970) 5(2):131–84.
6.
The Japan Society for Transplantation. Summary of Clinical Registration of Kidney Transplantation (1990). Jpn J Transpl (1991) 26(5):494–517.
7.
The Japan Society for Transplantation. Fact Book 2024 on Organ Transplantation in Japan. Available online at: https://www.asas.or.jp/jst/pdf/factbook/factbook2024.pdf (Accessed October 5, 2025).
8.
Masaki T Hanafusa N Abe M . 2023 Annual Dialysis Data Report, JSDT Renal Data Registry. J Jpn Soc Dial Ther (2024) 57(12):543–620. 10.4009/jsdt.57.543
9.
Terunuma Y Mathis BJ . Cultural Sensitivity in Brain Death Determination: A Necessity in End-of-Life Decisions in Japan. BMC Med Ethics (2021) 22(1):58. 10.1186/s12910-021-00626-2
Summary
Keywords
dialysis, kidney failure, kidney replacement therapy, kidney translant, kidney transplantation
Citation
Komaba H, Nakagawa Y, Koizumi M, Tomita Y and Nakamura M (2025) Estimated Number of Prevalent Kidney Transplant Recipients in Japan From 1964 to 2023. Transpl. Int. 38:15732. doi: 10.3389/ti.2025.15732
Received
14 October 2025
Revised
24 November 2025
Accepted
05 December 2025
Published
15 December 2025
Volume
38 - 2025
Updates
Copyright
© 2025 Komaba, Nakagawa, Koizumi, Tomita and Nakamura.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hirotaka Komaba, hkomaba@tokai.ac.jp
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.