Dear Editors,
Immunoglobulin G4-related disease (IgG4-RD) is a systemic fibroinflammatory disorder characterized by tumefactive lesions, storiform fibrosis, and a dense lymphoplasmacytic infiltrate enriched in IgG4-positive plasma cells [1]. Cutaneous involvement is uncommon (approximately 4%–6%) and typically presents as erythematous plaques or subcutaneous nodules on the head and neck [1, 2]. Reports of scarring alopecia associated with IgG4-RD are limited. We herein describe a young Japanese man with scalp IgG4-RD clinically mimicking acne keloidalis nuchae (AKN), in whom alopecia was caused by dermal fibrosis rather than follicular inflammation.
A 23-year-old Japanese man first noticed a small papule on his occipital scalp in his late teens, which gradually enlarged over several years. At presentation, he had a 5 × 3 cm indurated erythematous plaque with scarring and alopecia on the occipital scalp (Figures 1a,b). The lesion was non-pruritic, non-painful, and showed no pustules or purulent discharge. He had no significant medical history. Laboratory testing showed an elevated serum IgG4 level (153 mg/dL; normal <135), and both serum IgE and peripheral eosinophil counts were within normal ranges. Computed tomography revealed no extracutaneous involvement. Histopathologic examination demonstrated dense dermal fibrosis with patchy islands of lymphoplasmacytic infiltrates (Figures 1c,d). Most infiltrating cells were plasma cells, with more than 200 IgG4-positive cells per high-power field and an IgG4/IgG ratio exceeding 40% (Figures 1e,f). Storiform fibrosis was evident, while keloidal collagen bundles, follicular abscesses, or neutrophilic infiltration typical of AKN were absent. Obliterative phlebitis was not seen. These findings fulfilled the comprehensive diagnostic criteria for IgG4-related disease, as proposed by Umehara et al. [3].
FIGURE 1
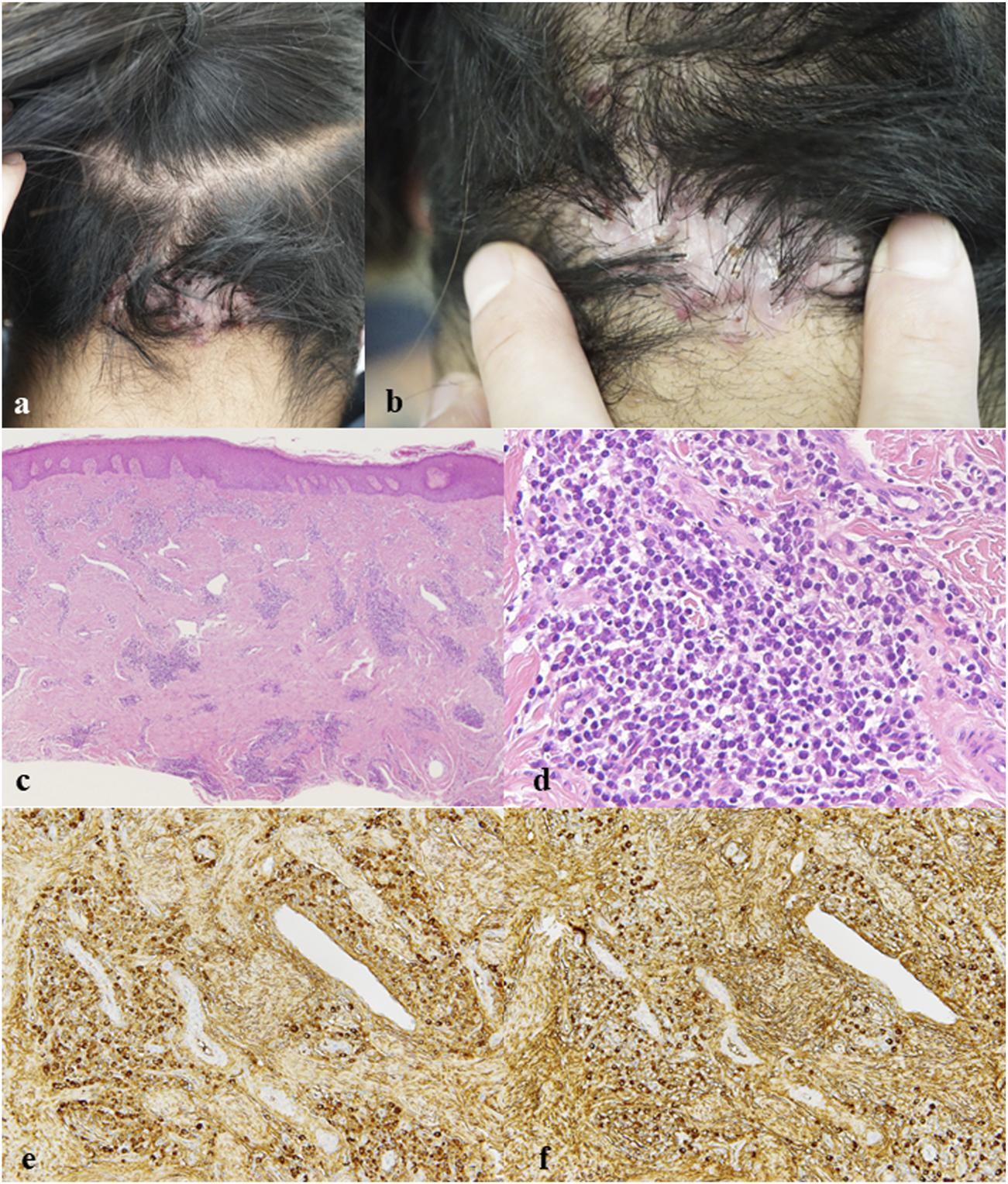
(a,b) Clinical features: An erythematous plaque with scarring and alopecia on the occipital scalp. (c) Hematoxylin and eosin (H&E), ×20: Patchy islands of lymphoplasmacytic infiltrates within the dermis. (d) H&E, ×400: Most infiltrating lymphocytes were plasma cells. (e) IgG immunostaining, ×200: Numerous IgG-positive plasma cells. (f) IgG4 immunostaining, ×200: The majority of IgG-positive plasma cells were IgG4-positive.
Clinically, the indurated plaque on the nuchal scalp closely resembled AKN, a chronic scarring folliculitis typically seen in young men of African or Asian descent [4]. Both conditions share a predilection for the occipital region and may present as firm fibrotic plaques associated with alopecia. However, AKN is fundamentally a perifollicular inflammatory process triggered by repeated mechanical irritation, friction, or follicular occlusion, leading to folliculitis and secondary fibrosis. In contrast, IgG4-RD represents a systemic fibroinflammatory condition characterized by Th2-dominant immune responses and regulatory T-cell activation, resulting in dense IgG4-rich plasma cell infiltration and fibrosis in multiple organs [5].
Several features favored IgG4-RD in this case: the absence of pustules, sinus tracts, or pain; uniform dermal fibrosis rather than keloidal collagen deposition; and a diffuse lymphoplasmacytic infiltrate rich in IgG4-positive plasma cells. Furthermore, the mildly elevated serum IgG4 level and storiform fibrosis pattern strongly suggested an IgG4-mediated process rather than post-inflammatory scarring. The histological composition—dominated by plasma cells and lacking folliculocentric inflammation—was inconsistent with classical AKN, even in its late fibrotic stage.
Cutaneous IgG4-RD accounts for only 4%–6% of systemic IgG4-RD cases and typically involves the head and neck region [1, 2]. Tokura et al., in a report published in British Journal of Dermatology (2014), described that cutaneous IgG4-related disease typically shows dense dermal fibrosis with lymphoplasmacytic infiltration rich in IgG4-positive plasma cells. Our case broadens this clinical spectrum by illustrating that IgG4-RD can closely mimic AKN both clinically and topographically while differing fundamentally in pathogenesis. To our knowledge, no previous reports have documented AKN-like lesions as a presentation of biopsy-proven IgG4-RD.
Therefore, careful diagnostic interpretation and long-term follow-up are warranted in this case. It remains controversial whether isolated cutaneous lesions truly represent a limited form of IgG4-related disease or whether some cases merely reflect localized fibrotic processes accompanied by reactive aggregation of IgG4-positive plasma cells. In the biopsy specimen, dense dermal fibrosis was present with only a few residual hair follicles, and no perifollicular inflammation was observed. Clinically, however, mild tufted hair was noted, suggesting prior perifollicular inflammation and follicular destruction. This finding does not exclude the possibility that earlier inflammatory changes had already regressed by the time of biopsy. Even in patients who initially present with solitary skin lesions, the potential for subsequent development of extracutaneous involvement cannot be completely excluded. Given that our patient was incidentally diagnosed by skin biopsy at a young age and showed no systemic lesions at that time, vigilant long-term surveillance is considered necessary.
The lesion was treated with intralesional triamcinolone injections, which resulted in mild improvement of erythema and induration, but alopecia persisted after 6 months. Although systemic corticosteroids are considered first-line therapy for IgG4-RD, localized disease may respond to intralesional therapy. Whether scarring alopecia in IgG4-RD is reversible remains unclear; however, early recognition and treatment may prevent irreversible fibrosis.
In summary, this patient presented with a nonpurulent, painless alopecic plaque in which histopathological findings and elevated serum IgG4 levels strongly suggested IgG4-related disease. However, the clinical presentation closely resembled acne keloidalis nuchae, a far more common condition that is usually diagnosed without biopsy. Given the rarity of isolated cutaneous IgG4-RD, the possibility that this lesion represents a localized fibrotic process with reactive IgG4-positive plasma cell infiltration cannot be completely excluded. Nonetheless, this case underscores the importance of considering IgG4-RD in the differential diagnosis of atypical cicatricial alopecia and highlights the value of IgG4 immunostaining in distinguishing it from more common scarring folliculitides or AKN.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
AS and TK collected the clinical data and prepared the clinical figures. SH conceived the study, performed the literature review, and drafted the manuscript. ST contributed to histopathological analysis and interpretation. KI supervised the study and critically revised the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declared that financial support was not received for this work and/or its publication.
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
References
1.
TakayamaRUenoTSaekiH. Immunoglobulin G4-related disease and its skin manifestations. J Dermatol (2017) 44:288–96. 10.1111/1346-8138.13723
2.
CharrowAImadojemuSStephenSOgunleyeTTakeshitaJLipoffJB. Cutaneous manifestations of IgG4-related disease: a systematic review. J Am Acad Dermatol (2016) 75:197–202. 10.1016/j.jaad.2016.01.046
3.
UmeharaHOkazakiKMasakiYKawanoMYamamotoMSaekiTet alA novel clinical entity, IgG4-related disease (IgG4RD): general concept and details. Mod Rheumatol (2012) 22:1–14. 10.1007/s10165-011-0508-6
4.
OgunbiyiA. Acne keloidalis nuchae: prevalence, impact, and management challenges. Clin Cosmet Investig Dermatol (2016) 9:483–9. 10.2147/CCID.S99225
5.
StoneJHZenYDeshpandeV. Mechanisms of disease: IgG4-related disease. N Engl J Med (2012) 366:539–51. 10.1056/NEJMra1104650
Summary
Keywords
acne keloidalis nuchae, alopecia, igg4, IgG4-related disease, plasma cell
Citation
Suwayama A, Kaminaga T, Hayashi S, Tokoro S and Igawa K (2026) Cicatricial alopecia of the scalp as a manifestation of IgG4-related disease mimicking acne keloidalis nuchae. J. Cutan. Immunol. Allergy 8:15953. doi: 10.3389/jcia.2025.15953
Received
26 November 2025
Revised
17 December 2025
Accepted
23 December 2025
Published
07 January 2026
Volume
8 - 2025
Updates
Copyright
© 2026 Suwayama, Kaminaga, Hayashi, Tokoro and Igawa.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shujiro Hayashi, shayashi@dokkyomed.ac.jp
ORCID: Shujiro Hayashi, orcid.org/0000-0001-6558-4818
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.