Abstract
We report a rare case of dermatomyositis in a woman in her 60s, presenting with chronic pruritic erythema and symmetrical subcutaneous indurations in both axillae. Physical examination revealed Gottron’s papules and erythematous plaques on the hands and upper extremities. Laboratory tests showed mildly elevated serum CK, aldolase, and CRP levels. CT revealed increased fat density in both axillae, suggestive of panniculitis. Skin and subcutaneous biopsies confirmed interface dermatitis and panniculitis with membranocystic changes. After that, bilateral inguinal panniculitis developed. Autoantibody screening identified strong positivity for anti-NXP-2 and anti-Ki antibodies. Anti-NXP-2 antibody was further confirmed by immunoprecipitation-Western blotting. The diagnosis of dermatomyositis was made, and oral prednisolone (10 mg, 0.2 mg/kg/day) led to marked improvement. These findings may suggest a potential association between anti-NXP-2 antibodies and panniculitis.
Introduction
Dermatomyositis is a rare autoimmune disorder characterized by inflammatory myopathy and distinctive skin rashes. Diagnosis can be challenging, and early recognition is crucial for appropriate management. Here, we present a case of dermatomyositis in a 60s female with skin findings, elevated CK levels, and positive anti-NXP-2 antibody.
Case description
A woman in her 60s presented with a 1-year history of erythematous and pruritic lesions on the trunk and extremities. She initially consulted a local dermatologist and was treated with anti-allergic agents and topical corticosteroids, with no improvement. Subsequently, she visited an internist, where blood tests revealed elevated serum CK levels. Suspecting dermatomyositis, she was referred to the Department of Hematology, Rheumatology, and Collagen Diseases, and later to our department for further dermatological evaluation.
Her medical history included hypothyroidism, familial hypercholesterolemia, and hypertension. She had no muscle weakness, joint pain, or Raynaud’s phenomenon. On physical examination, she had Gottron’s papules and erythematous plaques with scaling and excoriation on the dorsum of the hands, upper arms, and elbows (Figures 1A,B). There was no periungual erythema or nailfold hemorrhage. During the disease course, she developed painful, symmetrical subcutaneous indurations in both axillae (Figure 1C).
FIGURE 1
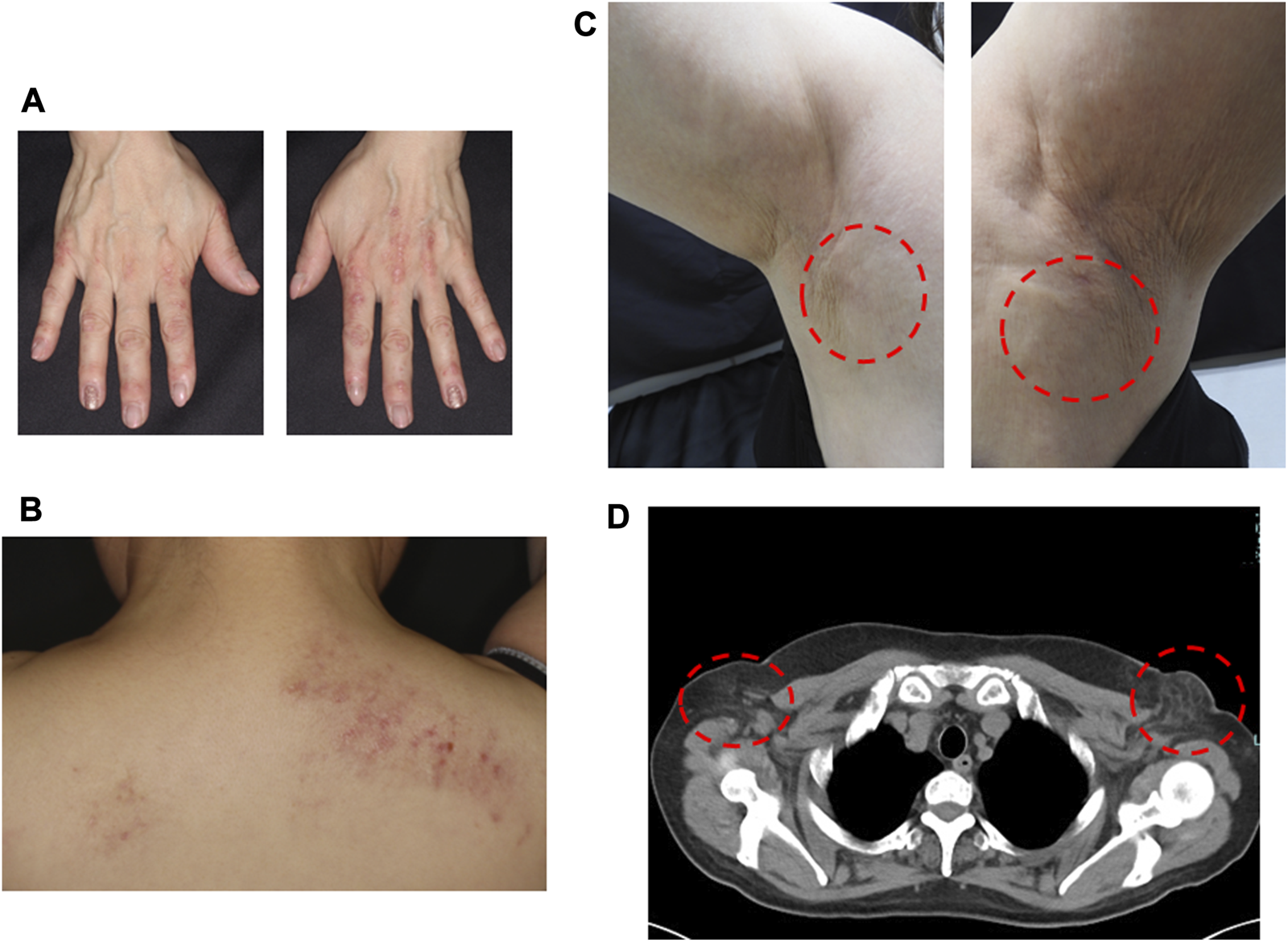
Clinical manifestations (A) Erythema and papule on the dorsal surface of the finger. (B) Erythema with a few scales and scrape marks on the back. (C) Symmetrical painful subcutaneous induration appeared in both axillae during the course of the disease. (D) CT showed increased adipose tissue density consistent with panniculitis in both axillae.
Laboratory tests revealed elevated levels of CK (204 U/L), aldolase (12.6 U/L), AST (108 U/L), ALT (188 U/L), γ-GTP (112 U/L), CRP (0.41 mg/dL), and TARC (358 pg/mL). ANA was positive (speckled pattern, titer 1:40). Autoantibodies including anti-Jo-1, anti-ARS, anti-MDA5, anti-Mi-2, anti-TIF1-γ, anti-Scl-70, anti-dsDNA, anti-ssDNA, anti-Sm, anti-RNP, anti-SSA, and anti-SSB were all negative. A plain computed tomography (CT) scan showed no evidence of interstitial pneumonia or malignancy. However, increased density of adipose tissue was noted in both axillae, consistent with panniculitis (Figure 1D). A-Cube® autoantibody array (Fushimi Pharmaceutical Co., Ltd.) revealed strong positivity for anti-NXP-2 antibody (865.0 Index) and anti-Ki antibody (135.9 Index). Immunoprecipitation-western blotting confirmed the presence of anti-NXP-2 antibodies (Supplementary Figure S1). Informed consent to publication was obtained.
Histopathological examination of a skin biopsy from the dorsum of the hand showed liquefactive degeneration at the dermo-epidermal junction, thickened collagen bundles in the dermis, and mucin-like deposition (Figure 2A). Biopsy of the axillary lesion revealed slight separation of collagen fibers in the dermis and a membranous cystic structure in subcutaneous fat and surrounding lymphocytic infiltrate, consistent with panniculitis. And lobular panniculitis in the subcutaneous tissue layer with cystic changes of the membrane, and adipocyte necrosis (Figure 2B).
FIGURE 2
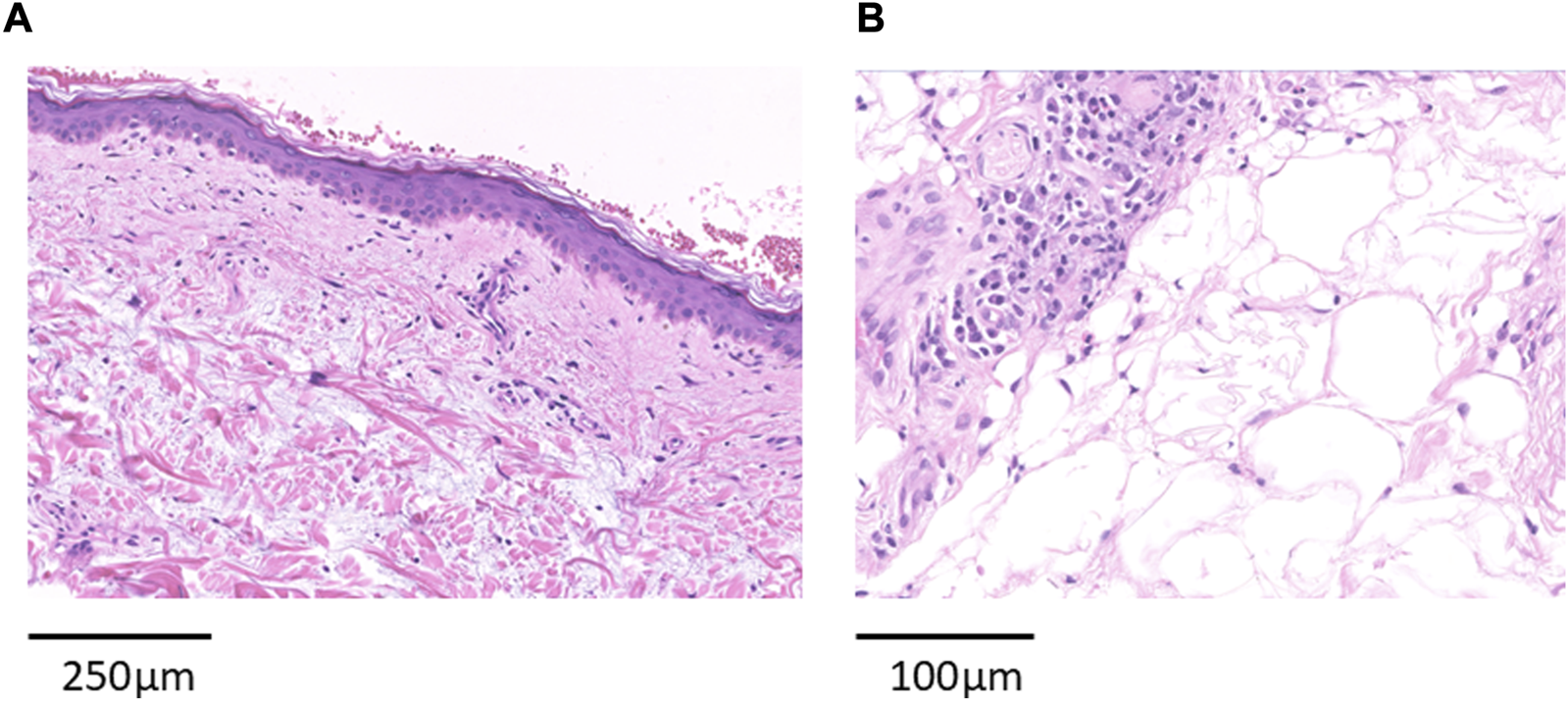
Histopathological Findings (A) Skin biopsy of erythema on the dorsal surface of the hands showed liquefactive degeneration at the epidermal-dermal interface, enlarged collagen fibers in the dermis, and mucin-like deposits (bar: 250 μm). (B) Skin biopsy of the subcutaneous induration in the axilla showed a membranocystic change and surrounding lymphocytic infiltrate was observed in the subcutaneous fat (bar: 100 μm).
The patient was initially treated with topical clobetasol propionate, oral olopatadine, and Bilastine for pruritic erythema. In the third month after the initial visit, panniculitis developed in both inguinal regions. In the fourth month, anti-NXP-2 antibody positivity confirmed the diagnosis of dermatomyositis. Oral prednisolone (10 mg, 0.2 mg/kg/day) was initiated, resulting in clinical improvement of both cutaneous and subcutaneous lesions (Figure 3).
FIGURE 3
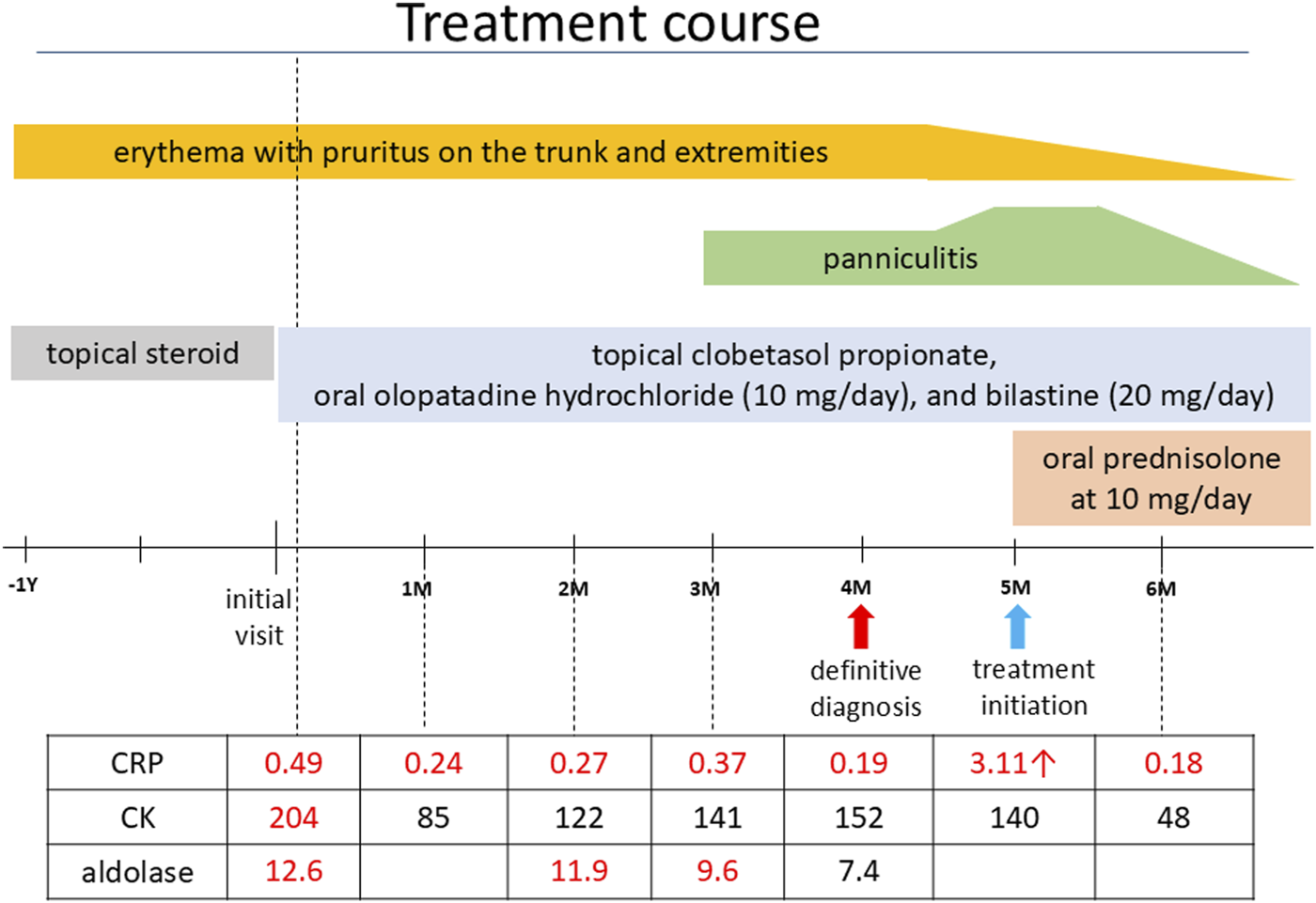
Treatment course. Treatment course, laboratory findings, and clinical improvement before and after the patient’s presentation.
Discussion
According to the revised diagnostic criteria of the Ministry of Health, Labor and Welfare (MHLW)1, this patient presented with Gottron’s papules and Gottron’s sign as cutaneous manifestations, mildly elevated levels of CK and aldolase, a mildly positive CRP level, and was positive for anti-NXP-2 antibody. Although these findings were consistent with dermatomyositis, the patient did not fully meet the diagnostic criteria in the established classification and was diagnosed with hypomyopathic dermatomyositis.
Recently Xie performed a retrospective study for clinical characteristics of 293 patients with dermatomyositis and revealed that 7.7% of the patients showed positive for anti-NXP-2 antibody. The clinical features of anti-NXP-2-positive dermatomyositis showed more symptoms of muscle involvement such as muscle weakness, muscle pain, dysphagia, and a lower probability of comorbid rashes than other antibodies [1]. In juvenile dermatomyositis, it is positive in 20%–30% of cases and is often associated with cutaneous calcification [2]. Ichimura et al. performed a multicentre retrospective observational study on 76 anti-NXP-2 antibody-positive patients. Adult patients with anti-NXP-2 antibody in that study tend to present polymyositis phenotype lacking dermatomyositis-specific skin manifestations (heliotrope rash or Gottron sign/papules) and 11.8% of the patients had subcutaneous calcinosis, and 26.3% had subcutaneous oedema [3].
Anti-Ki antibodies, first reported by Tojo et al. in 1980 in the sera of patients with systemic lupus erythematosus [4], target the nuclear protein PSME3 (proteasome activator complex subunit 3). Anti-Ki antibodies have also been reported as autoantibodies to Ki/SL and are considered biomarkers for systemic lupus erythematosus and sicca syndrome [5]. As far as we searched for, there have been only one patient a systemic sclerosis/dermatomyositis overlap patient presenting with anti-Ku and anti-Ki antibodies [6]. It remains unclear how the presence of this anti-Ki antibody is related to dermatomyositis with extensive panniculitis, as seen in this case. Further accumulation of cases is needed.
Panniculitis is an inflammation of the subcutaneous adipose tissue and is characterized by indurated, painful, and erythematous subcutaneous nodules commonly located on the thighs, arms, and buttocks. These nodules can progress to calcifications and lipoatrophy [7]. From 1985 to 2025 in Japan, 33 cases of dermatomyositis complicated by panniculitis (including autopsy cases) were identified, with a mean age of 47 years and a male-to-female ratio of 5:28. The lesions were predominantly located on the limbs and trunk. There were three reported cases of panniculitis involving the axillae, including autopsy cases. Antinuclear antibody positivity was observed in 17 patients, and only the autopsy case was positive for anti-NXP-2 antibodies. Interstitial pneumonia was present in approximately 30% of cases. Muscle symptoms were observed in some patients, and 23 received prednisolone (PSL) at doses of 30 mg or higher. Treatment response was generally favorable, with mortality primarily attributable to interstitial pneumonia (Supplementary Table S1). Interestingly, a recent published international review has found panniculitis in 16 (7.8%) of 205 patients with dermatomyositis. Among these, 9 (56.3%) tested positive for anti-NXP-2 antibodies, suggesting a potential association between anti-NXP-2 antibody positivity and panniculitis [8]. However, in one study of 91 patients with dermatomyositis associated panniculitis reported 3.3% for anti-NXP-2 antibody [9]. Further accumulation of cases is needed in the future.
Similar cases have previously been reported. One of the case showed symmetrical panniculitis of in dermatomyositis patient but autoantibody of the case is unclear [10]. The other similar case a 20-year-old woman who developed heliotrope rash and muscle weakness 2 years prior. Five months before presentation, panniculitis appeared in her extremities. She was positive for anti-NXP-2 antibodies, and her CK was markedly elevated at 15,316 U/L. Histopathological examination revealed lobular fat necrosis and calcification. She was initially treated with PSL 10 mg/day, but relapsed, requiring methylprednisolone pulse therapy (1,000 mg/day for 3 days), followed by PSL 40 mg/day and methotrexate 10 mg/week. Residual nodules were noted to slightly regress over time [11]. In comparison with the previously reported cases, the present case exhibited several distinctive features. Whereas marked elevations in CK levels and muscle weakness were commonly observed in prior reports, our patient showed only mild CK elevation without muscle weakness. Moreover, subcutaneous calcification, frequently reported in association with panniculitis in dermatomyositis, was absent. Treatment approaches also differed. In previous cases, high-dose glucocorticoids were administered to manage significant myositis symptoms. By contrast, in the present case, prednisolone was initiated at a low dose of PSL10mg (0.2 mg/kg/day), reflecting the predominance of cutaneous findings and the patient’s refusal of hospitalization. Nevertheless, due to the slow resolution of panniculitis, tacrolimus was subsequently introduced. These clinical differences suggest that panniculitis associated with dermatomyositis may present with heterogeneous severity and therapeutic responses, emphasizing the need for individualized treatment strategies.
We herein report a case of dermatomyositis complicated by lipodystrophy in both axillae and inguinal regions, with simultaneous detection of anti-NXP-2 and anti-Ki antibodies using the A-Cube®. Immunoprecipitation-Western blotting confirmed the presence of anti-NXP-2 antibodies. Given the rarity of dermatomyositis cases with concurrent panniculitis and anti-NXP-2 antibody positivity, further accumulation and analysis of similar cases are warranted to better understand their clinical characteristics and outcomes.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the studies involving humans because this is just a case repot. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
EU and AS wrote the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The authors declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontierspartnerships.org/articles/10.3389/jcia.2025.15763/full#supplementary-material
Footnotes
1.^chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/0000089962.pdf
References
1.
XieXDaiXLiuHXingY. A retrospective study for clinical characteristics of 293 patients with dermatomyositis. Medicine (Baltimore) (2024) 103(46):e40605. 10.1097/MD.0000000000040605
2.
IshikawaAMuroYSugiuraKAkiyamaM. Development of an ELISA for detection of autoantibodies to nuclear matrix protein 2. Rheumatology (Oxford) (2012) 51(7):1181–7. 10.1093/rheumatology/kes033
3.
IchimuraYKonishiRShoboMInoueSOkuneMMaedaAet alAnti-nuclear matrix protein 2 antibody-positive inflammatory myopathies represent extensive myositis without dermatomyositis-specific rash. Rheumatology (Oxford) (2022) 61(3):1222–7. 10.1093/rheumatology/keab518
4.
TojoTKaburakiJHayakawaMOkamotoTTomiiMHommaM. Precipitating antibody to a soluble nuclear antigen “Ki” with specificity for systemic lupus erythematosus. Ryumachi (1981) 21(Suppl. l):129–40. Available online at: https://www.ncbi.nlm.nih.gov/pubmed/6979801.
5.
MahlerMBentowCAureMAFritzlerMJSatohM. Significance of autoantibodies to Ki/SL as biomarkers for systemic lupus erythematosus and sicca syndrome. J Clin Med (2022) 11(12):3529. 10.3390/jcm11123529
6.
MiyachiKHankinsRWMimoriTOkanoYAkizukiM. Prospective study of a systemic sclerosis/dermatomyositis overlap patient presenting with anti-Ku and anti-Ki antibodies. Mod Rheumatol (2002) 12(3):253–5. 10.3109/s101650200045
7.
DouvoyiannisMLitmanNDulauAIlowiteNT. Panniculitis, infection, and dermatomyositis: case and literature review. Clin Rheumatol (2009) 28(Suppl. 1):S57–63. 10.1007/s10067-009-1160-9
8.
XingX-JWangSLiA-QLiZ-HLinB-W. Panniculitis, an uncommon skin manifestation in adult dermatomyositis. Int J Dermatol Venerology (2023) 6(2):96–101. 10.1097/JD9.0000000000000260
9.
HoJDMcKenzieT. Panniculitis in dermatomyositis: a systematic review of the clinicopathologic features. JAAD Internatoinal (2025) 18:50–61. 10.1016/j.jdin.2024.03.004
10.
FornaroMCarlinoGAbbruzzeseAPiccinniARIannoneF. Symmetrical panniculitis in a patient with dermatomyositis: an unusual onset. J Clin Rheumatol (2020) 26(8):e311. 10.1097/RHU.0000000000001164
11.
van DongenHMvan VugtRMStoofTJ. Extensive persistent panniculitis in the context of dermatomyositis. J Clin Rheumatol (2020) 26(6):e187–e188. 10.1097/RHU.0000000000001058
Summary
Keywords
dermatomyositis, anti-NXP-2 antibody, anti-Ki antibody, panniculitis, A-cube®
Citation
Uchiyama E, Tochigi M, Takamiya Y, Shimizu A, Matsushita T and Yamada K (2025) Case Report: Dermatomyositis with symmetrical axillary and inguinal panniculitis associated with anti-NXP-2. J. Cutan. Immunol. Allergy 8:15763. doi: 10.3389/jcia.2025.15763
Received
19 October 2025
Revised
09 November 2025
Accepted
20 November 2025
Published
01 December 2025
Volume
8 - 2025
Updates
Copyright
© 2025 Uchiyama, Tochigi, Takamiya, Shimizu, Matsushita and Yamada.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Akira Shimizu, ashimizu@kanazawa-med.ac.jp
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.