Dear Editors,
Generalized pustular psoriasis (GPP) is a rare and life-threatening subtype of psoriasis characterized by recurrent flares, systemic inflammation, and sterile pustules [1]. Accurate biomarkers that reflect disease activity and treatment response are needed in clinical practice. The neutrophil percentage-to-albumin ratio (NPAR) is an emerging inflammatory marker that reflects both immune activation and nutritional status [2]. However, its relevance in GPP remains poorly understood.
This retrospective study aimed to evaluate the clinical utility of NPAR in GPP by comparing NPAR values among patients with GPP, psoriasis vulgaris (PsV), psoriatic arthritis (PsA), and healthy controls (HC). We also examined longitudinal changes in NPAR before and after treatment in GPP, and assessed its correlation with the generalized pustular psoriasis area and severity index (GPPASI) or with C-reactive protein (CRP), and the Severity Score for GPP.
Patients diagnosed with GPP at the University of Tokyo Hospital between January 2017 and March 2025 were included. Patients with PsV, PsA, and healthy controls were enrolled based on their initial visits occurring between January 2024 and March 2025. All diagnoses were made by dermatologists and rheumatologists. Patients with GPP complicated by infection were excluded. Laboratory data were collected at peak disease activity (initial visit or during hospitalization) for GPP, and at first visit for PsV, PsA, and HC. NPAR was calculated using the following formula: NPAR = Neutrophil percentage [%]/Albumin level [g/dL]. Post-treatment NPAR in GPP patients was derived from laboratory data collected approximately 3 months after therapy initiation. The medical ethics committee of the University of Tokyo approved all described studies (No. 3360), and the study was conducted according to the principles of the Declaration of Helsinki.
A total of 124 subjects were included: 13 GPP, 44 PsV, 37 PsA, and 30 HC. The GPP group consisted of 4 males and 9 females, with a median age of 58 years (range: 22–73), including 12 Japanese and 1 Chinese patient. NPAR values were significantly elevated in GPP patients compared to those with PsV (p = 0.0046), PsA (p = 0.0048), and HC (p = 0.0016), as determined by Kruskal–Wallis test followed by Dunn–Bonferroni post hoc test (Figure 1A). Further analyses were conducted to assess the impact of treatment on NPAR values within the GPP group. Post-treatment NPAR values significantly decreased compared to pre-treatment levels, as evaluated using Wilcoxon matched-pairs signed-rank test (p = 0.021; Figure 1B). We also evaluated potential correlations between NPAR and other relevant clinical indicators. The analysis revealed a strong positive correlation between NPAR and the GPPASI (r = 0.8636, p = 0.0012, n = 11; Figure 1C). A similarly strong positive correlation was observed between NPAR and CRP levels (r = 0.8352, p = 0.0007, n = 13; Figure 1D). In addition, NPAR also correlated strongly with the Severity Score (r = 0.8695, p = 0.0009, n = 11; Figure 1E).
FIGURE 1
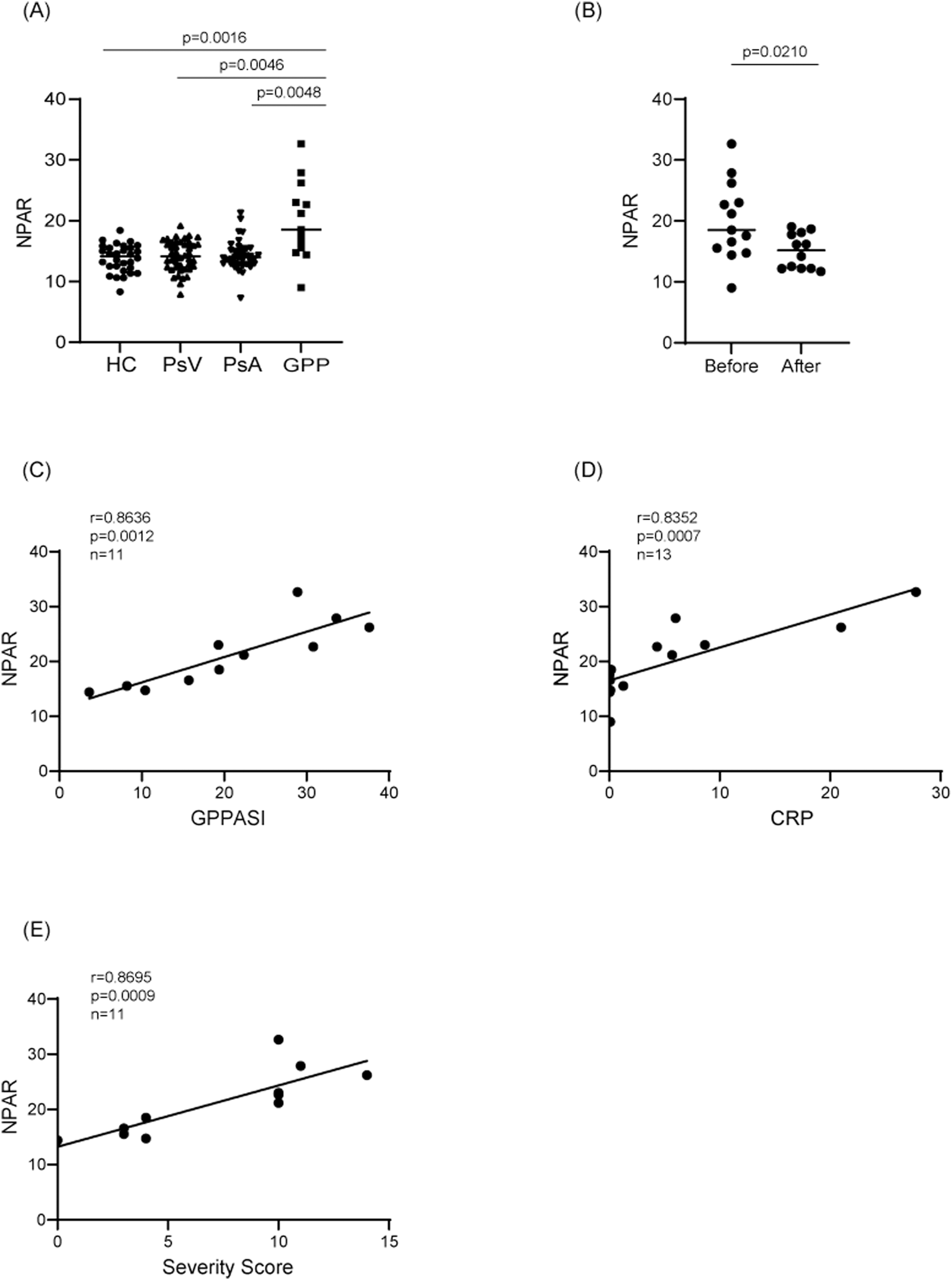
Comparative and correlative analysis of NPAR in psoriasis patients. (A) NPAR comparison among patients with generalized pustular psoriasis (GPP), psoriasis vulgaris (PsV), psoriatic arthritis (PsA), and healthy controls (HC). Statistical analysi s was performed using Kruskal–Wallis test followed by Dunn–Bonferroni post hoc test. (B) Changes in NPAR values in GPP patients before and after treatment. Statistical significance was evaluated by Wilcoxon matched-pairs signed-rank test. (C–E) Correlation analyses between NPAR and clinical indicators in patients with GPP. Correlations of NPAR with (C) Generalized Pustular Psoriasis Area and Severity Index (GPPASI) scores (D) C-reactive protein (CRP) levels, and (E) Severity Score for GPP are demonstrated. Solid lines represent linear regression fits. Correlation strength was assessed using Spearman’s rank correlation coefficient (r).
The significant elevation of NPAR observed in GPP patients aligns well with current understanding of the pathogenic mechanisms involving neutrophil activation [3]. Moreover, the inclusion of albumin levels in NPAR calculation offers additional clinical relevance. Given that lower albumin levels in GPP primarily result from increased vascular permeability associated with systemic inflammation [4, 5]. Capillary leak syndrome, a complication of GPP, may reflect the most severe clinical manifestation of this pathophysiology and is characterized by prominent edema, which can lead to respiratory failure and circulatory collapse [1]. Therefore, the combination of neutrophil percentage and albumin in NPAR provides a comprehensive assessment of both inflammatory and vascular factors, thereby enhancing its clinical interpretability and applicability.
The study further highlights the responsiveness of NPAR to therapeutic intervention. The significant reduction in NPAR post-treatment suggests its potential utility in monitoring therapeutic responses and disease progression. Given the observed NPAR changes correlating with clinical improvements, NPAR may offer clinicians a valuable tool for evaluating treatment effectiveness in real-time, aiding clinical decision-making and patient management.
Limitations of this study include its retrospective design and relatively small sample size. Future prospective studies with larger cohorts are necessary to validate these findings and explore the predictive capabilities of NPAR regarding long-term disease outcomes.
In conclusion, NPAR emerges as a promising biomarker that combines inflammatory and vascular indicators, strongly correlating with disease severity and systemic inflammation in GPP.
Statements
Data availability statement
The datasets generated and/or analyzed in the current study contain human clinical information and are not publicly available due to ethical restrictions. However, de-identified data may be made available from the corresponding author on reasonable request.
Ethics statement
The studies involving humans were approved by the institutional review board of the University of Tokyo. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because the study involved retrospective analysis of existing data, and participants were provided the opportunity to opt-out. The waiver was approved by the Institutional Review Board.
Author contributions
AY and SaS designed the experiments and wrote the manuscript. AY collected the patients’ data. AY analyzed the data, with contributions from SaS and ShS supervised the project. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by grants from the Ministry of Education, Culture, Sports, Science and Technology of Japan (24K11447).
Conflict of interest
SaS received honoraria for lectures from Maruho, AbbVie, Kyowa Kirin, Eli Lilly, Janssen Pharmaceutical, Boehringer Ingelheim, Sun Pharma, and LEO Pharma. The funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. During the preparation of this work the author used DeepL in order to improve readability and language. After using this tool, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
References
1.
FujitaHTeruiTHayamaKAkiyamaMIkedaSMabuchiTet alJapanese guidelines for the management and treatment of generalized pustular psoriasis: the new pathogenesis and treatment of GPP. J Dermatol (2018) 45(11):1235–70. 10.1111/1346-8138.14523
2.
GongYLiDChengBYingBWangB. Increased neutrophil percentage-to-albumin ratio is associated with all-cause mortality in patients with severe sepsis or septic shock. Epidemiol Infect (2020) 148:e87. 10.1017/S0950268820000771
3.
ShaoSFangHZhangJJiangMXueKMaJet alNeutrophil exosomes enhance the skin autoinflammation in generalized pustular psoriasis via activating keratinocytes. FASEB J (2019) 33(6):6813–28. 10.1096/fj.201802090RR
4.
AmanJvan der HeijdenMvan LingenAGirbesARvan Nieuw AmerongenGPvan HinsberghVWet alPlasma protein levels are markers of pulmonary vascular permeability and degree of lung injury in critically ill patients with or at risk for acute lung injury/acute respiratory distress syndrome. Crit Care Med (2011) 39(1):89–97. 10.1097/CCM.0b013e3181feb46a
5.
WatanabeAKamataMShimizuTUchidaHSakuraiESuzukiSet alSerum levels of angiogenesis-related factors in patients with psoriasis. J Dermatol (2023) 50(2):222–8. 10.1111/1346-8138.16588
Summary
Keywords
generalized pustular psoriasis, neutrophil, albumin, NPAR, psoriasis
Citation
Yoshimura A, Sato S and Shibata S (2025) Association between the neutrophil percentage-to-albumin ratio and generalized pustular psoriasis. J. Cutan. Immunol. Allergy 8:15227. doi: 10.3389/jcia.2025.15227
Received
05 July 2025
Accepted
01 August 2025
Published
11 August 2025
Volume
8 - 2025
Updates
Copyright
© 2025 Yoshimura, Sato and Shibata.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sayaka Shibata, shibatas-der@h.u-tokyo.ac.jp
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.