Dear Editors,
Pyoderma gangrenosum (PG) is often associated with hematological disorders such as leukemia, monoclonal gammopathy, and myelodysplastic syndrome. However, association of PG with aplastic anemia is rare. We experienced a patient with PG-associated aplastic anemia.
A 90-year-old Japanese woman had a painful subcutaneous induration on her mons pubis for 2 months and underwent a biopsy elsewhere. Only nonspecific inflammatory infiltrates in the adipose tissue were revealed. The biopsy site gradually ulcerated and multiple ulcers were observed. She was referred to our department for evaluation of the skin ulcers 10 days after the biopsy (Figure 1A). At her first visit, she was receiving prednisolone (PSL) (5 mg/day) and cyclosporine (CyA) (150 mg/day) for aplastic anemia, which was diagnosed 6 years earlier. As Escherichia coli (E. Coli) was detected in the wound, we initiated the administration of oral minocycline and topical anti-ulcer ointment. Moreover, we also reduced the dose of PSL to 3 mg/day and discontinued CyA considering the possibility of secondary wound infection in the immunosuppressed patient. However, the ulcer persisted and further enlarged centrifugally and fused to form a large ulcer in 3 months (Figure 1B). We performed a biopsy again of the ulcer edge, which revealed a deep ulcer and dense infiltration of neutrophils, lymphocytes, and histiocytes throughout the dermis (Figures 1C, D). Her red blood cell, white blood cell, and platelet counts were 235 × 104/μL, 6.9 × 103/μL, and 242 × 103/μL, respectively, and her CRP was 2.5 mg/dL. Based on the clinical and histological findings, a diagnosis of PG was made. Additionally, the dose of PSL was increased to 20 mg/day and CyA was restarted with only a limited effect. Adalimumab was administered, and the ulcer began to shrink. However, the drug was discontinued after one administration because of cytomegalovirus infection. She started to receive oral ganciclovir and PSL and CyA were discontinued due to the cytomegalovirus infection. She was transferred to another hospital and the wound continues to grow because PSL and CyA were not given. Since the cytomegalovirus infection is still present, adalimumab was not been restarted.
FIGURE 1
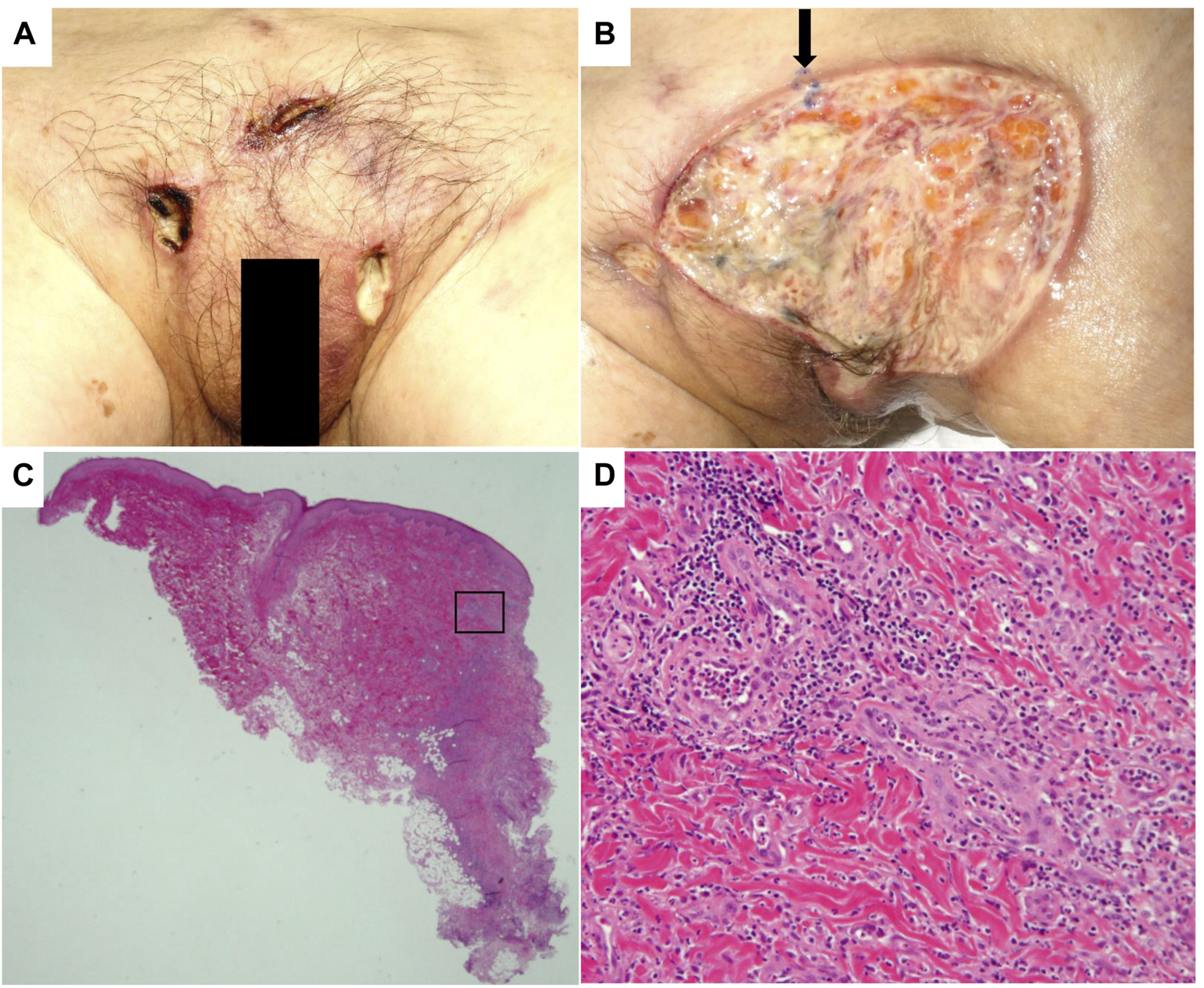
(A) Clinical finding of the patient’s ulcers at the first visit to our department. A total of three skin ulcers were observed on the pubic area. (B) The clinical finding 3 months after the first visit; skin ulcers have enlarged and fused to form a large ulcer. The arrow indicates the biopsy site. (C) Histopathology demonstrates ulcers extending into the subcutaneous fat tissue. The right edge of the tissue is the ulcer. (D) Infiltration of neutrophils and lymphocytes is observed around the base of the ulcer [Hematoxylin–eosin, original magnifications: ×12.5 (C), ×200 (D)].
PG is a rare inflammatory skin disorder characterized clinically by painful ulcers with necrotic surfaces and histologically by dense infiltration of neutrophils. The condition is often associated with systemic comorbidities, including inflammatory bowel disease, rheumatoid arthritis, aortitis syndrome, and hematological disorders. Anemia has been reported in patients [1]. Iron deficiency anemia is associated with the highest incidence [1]. Our review of previous literature revealed three cases of hemolytic anemia (such as Evans syndrome) [2] and three cases of Fanconi anemia (congenital aplastic anemia) [3] associated with PG, but no cases of acquired aplastic anemia were observed. In previous reports, the onset of hematological disorders preceded that of PG in most cases [3]. In our patient, aplastic anemia preceded the exacerbation of ulcers, which occurred after a reduction in the aplastic anemia treatment. This strongly suggested a connection between her aplastic anemia and the development of PG.
Approximately 70% of PG develops in the lower extremities, and PG in private areas is rare. Satoh et al. described two cases of genital PG and reported that systemic complications were rare in patients with genitalia-localized PG, based on a review of published work on Japanese cases [4]. As the number of cases with genitalia-localized PG is limited, further accumulation of such cases is needed. Diagnosticians should be aware of PG in patients with intractable skin ulcers associated with hematological malignancies.
Statements
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
AY, KF, and TK wrote the manuscript, AB and HK significantly contributed to data analysis and interpretation. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
PatelSHijazBNambudiriVE. Anaemia as a comorbidity in pyoderma gangrenosum hospitalizations. Exp Dermatol (2023) 33:e14925. 10.1111/exd.14925
2.
YangDHYangMY. Scrotal pyoderma gangrenosum associated with Evans syndrome. J Clin Med (2018) 7:230. 10.3390/jcm7090230
3.
MokrzyckiALheureCFranckNSociéGMauppinCde FontbruneFSet alPyoderma gangrenosum revealing myeloid activation of Fanconi anaemia: two case reports. Acta Derm Venereol (2020) 100:adv00338. 10.2340/00015555-3671
4.
SatohMYamamotoT. Genital pyoderma gangrenosum: report of two cases and published work review of Japanese cases. J Dermatol (2013) 40:840–3. 10.1111/1346-8138.12252
Summary
Keywords
aplastic anemia, hematological neoplasms, pubic area, pyoderma gangrenosum, skin ulcer
Citation
Yoshizaki A, Fujii K, Baba A, Kawada H and Kanekura T (2024) Pyoderma gangrenosum of the mons pubis associated with aplastic anemia. J. Cutan. Immunol. Allergy 7:12845. doi: 10.3389/jcia.2024.12845
Received
14 February 2024
Accepted
26 March 2024
Published
08 April 2024
Volume
7 - 2024
Updates
Copyright
© 2024 Yoshizaki, Fujii, Baba, Kawada and Kanekura.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ai Yoshizaki, k4234606@kadai.jp
ORCID: Ai Yoshizaki, orcid.org/0000-0003-0144-1345
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.