Dear Editors,
BK virus (BKV), present in 80%–90% of the population, establishes a lifelong persistent infection in the kidney and urinary tract after a subclinical primary infection. It can reactivate and cause de novo infection in immunocompromised kidney transplant recipients (KTRs) lacking neutralizing antibodies against the donor strain [1], causing nephropathy (BKVAN) in 4%–8% of cases. Persistent BKV infection increases the risk of urothelial carcinoma and collecting duct carcinoma (CDC) [2].
A 73-year-old KTR was admitted for asthenia, acute kidney injury (creatinine 320 μmol/L), inflammatory syndrome (CRP 130 mg/L), and anaemia (Hb 75 g/L). He was followed for a KT performed 9 years earlier, complicated by biopsy-proven BKVAN at month 10. Mycophenolate mofetil was switched to everolimus (3–8 ng/mL), then to leflunomide, and tacrolimus to ciclosporin (80–120 ng/mL). The viral load decreased over 5 months and BKV was never detected again in the blood. At admission, MRI revealed a hypovascular mass in the graft with central necrosis and retroperitoneal inflammation. Biopsy confirmed a tumour composed of irregular tubular structures, trabeculae and single cells (Figure 1). The nuclei had a high mitotic index. Necrotic changes were observed. This tumour proliferation infiltrated between non-tumour and dysplastic premalignant tubules (Figure 1A). Immunohistochemistry showed diffuse positivity of tumour cells for PAX8, CK7, INI1, fumarate hydratase, and SDHB, and focal positivity for GATA3 (Figure 1B), but negativity for CK20, p504S, p63, or ALK. Only tumour cells showed strong nuclear staining with anti-SV40 large T-antigen (Figure 1C), leading to the diagnosis of BKV-associated CDC. No metastases were initially found, and transplantectomy was performed. On pathological examination, the tumour invaded the surgical margins of the transplantectomy. Immunosuppressive therapy was tapered by withdrawing leflunomide and reducing tacrolimus trough levels, but not entirely discontinued in order to minimize the risk of donor-specific alloimmunization. Two months later, PET/CT showed iliac, retroperitoneal, pelvic lymph node metastases, and a right ischiopubic bone metastasis. Bulk HLA genotyping of the biopsy revealed that the tumour was not of recipient origin. Immunosuppression was completely withdrawn to stimulate the allo-immune anti-tumoral response, and the patient achieved complete metastatic regression within 3 months. At 2 years, he remained recurrence-free.
FIGURE 1
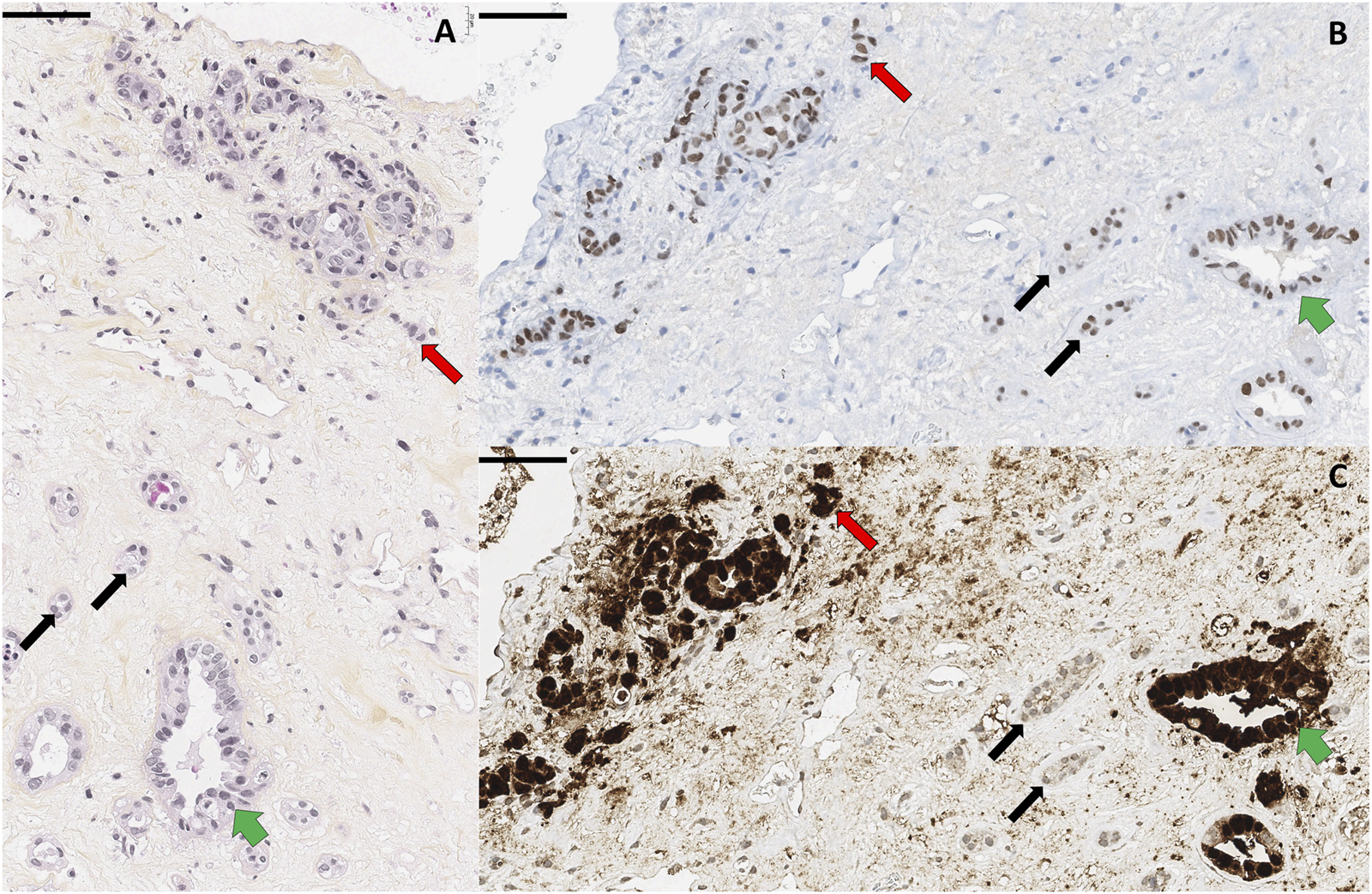
Pathological findings. (A) Haematoxylin-Eosin-Safran staining showing infiltrative carcinomatous cells (red arrows), dysplastic premalignant (green arrows) and normal (black arrows) renal tubules. (B,C) Immunohistochemical examinations showing PAX8 [renal origin, (B)] and Sv40 [viral antigen, (C)] labelling of the tumour. Scale bars 60 µm.
This is a very rare case of metastatic donor-derived BKV-induced CDC in a KTR, successfully managed without chemotherapy nor immunotherapy. Bellini’s CDC is a rare (<1%) and aggressive variant of renal cell carcinoma [2]. It has been hypothesized that CDC could be linked to BKV in transplanted patients [3]. No other specific risk factor have been identified. The tumorigenesis induced by BKV is known. Polyomaviruses encode 2 viral oncogenes, the small and the large T-antigen [4, 5]. They can inactivate tumour suppressor genes p53 and pRb. Deletion of p53 and pRB leads to gene instability and replication errors that contribute to oncogenesis. Dysregulation of large T-antigen, with persistent over-expression in non-lytic cells, promotes cell growth, genetic instability and neoplasic transformation [6, 7]. The high levels of large T-antigen expression in tumour nuclei is visualized by SV40 staining in immunohistochemistry. Microdissected samples of neoplasic cells usually contain DNA sequences specific for segments of BK-polyomavirus large T-antigen and VP1 genes. On the contrary, no BKV DNA sequences are detected in microdissected normal renal parenchyma [8]. Donor-derived tumours in KTRs are rare (<0.1%) and may arise from donor cells predisposed to oncogenesis. Key oncogenic drivers occur as early as late childhood and early adolescence. Then, late events during transplantation and under immunosuppression, such as BKV infection and genomic integration, may promote further oncogenesis in donor renal cells [9]. These donor-derived tumours offer a unique treatment opportunity: withdrawal of immunosuppression led to spontaneous alloimmune tumour rejection by enabling the immune system to target the graft through alloimmune and antitumour responses. Ortega et al reported remission of a metastatic donor-derived urothelial tumour after transplantectomy and immunosuppression withdrawal [10]. Meier et al achieved similar success in a metastatic Bellini carcinoma by boosting the anti-tumour immune response with IL-2 immunotherapy [3] (Supplementary Table S1).
This case highlights the specificity of urological tumours in KTRs. Identifying donor-derived malignancies may refine treatment strategies, reducing reliance on aggressive therapies. The clinical history reported in this case suggests pragmatic management, although this is by no means a recommendation. Firstly, given the very unfavourable prognosis of these tumours, it seems legitimate to perform surgery and completely stop immunosuppression. The two expected benefits of surgery are the removal of the largest possible tumour mass, and the avoidance of symptomatic toxic graft rejection. The addition of immunotherapy or chemotherapy should be discussed on a case-by-case basis, after evaluating the efficacy of the initial treatment. Given BKV’s oncogenic potential, long-term monitoring should extend beyond the risk of nephropathy to include surveillance for malignancy. Options could include annual urinary cytology screening, early invasive urological evaluation in the event of haematuria and potentially biannual imaging of the graft.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
FL and XC were responsible for data collection and interpretation and drafting the article. FL and XC generated the figure. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontierspartnerships.org/articles/10.3389/ti.2025.14664/full#supplementary-material
SUPPLEMENTARY TABLE S1table summarizing post-transplant CDC cases linked to BK virus.
References
1.
Solis M Velay A Porcher R Domingo-Calap P Soulier E Joly M et al Neutralizing Antibody-Mediated Response and Risk of BK Virus-Associated Nephropathy. J Am Soc Nephrol Janv (2018) 29(1):326–34. 10.1681/ASN.2017050532
2.
Dao M Pécriaux A Bessede T Dürrbach A Mussini C Guettier C et al BK virus-associated Collecting Duct Carcinoma of the Renal Allograft in a kidney-pancreas Allograft Recipient. Oncotarget. 13 mars (2018) 9(19):15157–63. 10.18632/oncotarget.24552
3.
Meier RPH Muller YD Dietrich PY Tille JC Nikolaev S Sartori A et al Immunologic Clearance of a BK virus-associated Metastatic Renal Allograft Carcinoma. Transplant 1 févr (2021) 105(2):423–9. 10.1097/TP.0000000000003193
4.
Wang Y Liu Y Deng W Fu F Yan S Yang H et al Viral Integration in BK polyomavirus-associated Urothelial Carcinoma in Renal Transplant Recipients: Multistage Carcinogenesis Revealed by next-generation Virome Capture Sequencing. Oncogene. 27 août (2020) 39(35):5734–42. 10.1038/s41388-020-01398-6
5.
Starrett GJ Yu K Golubeva Y Lenz P Piaskowski ML Petersen D et al Evidence for virus-mediated Oncogenesis in Bladder Cancers Arising in Solid Organ Transplant Recipients. Éditeur Elife 24 Mars (2023) 12:e82690. 10.7554/eLife.82690
6.
Kenan DJ Mieczkowski PA Burger‐Calderon R Singh HK Nickeleit V . The Oncogenic Potential of Bk‐Polyomavirus Is Linked to Viral Integration into the Human Genome. J Pathol (2015) 237(3):379–89. 10.1002/path.4584
7.
Tognon M Corallini A Martini F Negrini M Barbanti-Brodano G . Oncogenic Transformation by BK Virus and Association with Human Tumors. Oncogene. 11 août (2003) 22(33):5192–200. 10.1038/sj.onc.1206550
8.
Papadimitriou JC Randhawa P Rinaldo CH Drachenberg CB Alexiev B Hirsch HH . BK Polyomavirus Infection and Renourinary Tumorigenesis. Am J Transpl févr (2016) 16(2):398–406. 10.1111/ajt.13550
9.
Mitchell TJ Turajlic S Rowan A Nicol D Farmery JHR O’Brien T et al Timing the Landmark Events in the Evolution of Clear Cell Renal Cell Cancer: Tracerx Renal. Cell. 19 avr (2018) 173(3):611–23.e17. 10.1016/j.cell.2018.02.020
10.
Michel Ortega RM Wolff DJ Schandl CA Drabkin HA . Urothelial Carcinoma of Donor Origin in a Kidney Transplant Patient. J Immunother Cancer (2016) 4:63. 10.1186/s40425-016-0167-4
Summary
Keywords
donor-derived carcinoma, BK virus BKPyV, BK virus derived carcinoma, alloimmune response, collecting duct carcinoma
Citation
Lefevre F, Benoit-Janin M, Seizilles-de-Mazancourt E, Matillon X, Buron F, Koenig A, Dubois V, Dietz M, Rouvière O, Morelon E, Thaunat O and Charmetant X (2025) BK Virus: Beyond Nephropathy Metastatic BK Virus-Induced, Donor-Derived Bellini’s Carcinoma in a Kidney Allograft Recipient: Boosting Rejection to Treat the Cancer. Transpl. Int. 38:14664. doi: 10.3389/ti.2025.14664
Received
23 March 2025
Accepted
21 July 2025
Published
31 July 2025
Volume
38 - 2025
Updates
Copyright
© 2025 Lefevre, Benoit-Janin, Seizilles-de-Mazancourt, Matillon, Buron, Koenig, Dubois, Dietz, Rouvière, Morelon, Thaunat and Charmetant.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xavier Charmetant, xavier.charmetant01@chu-lyon.fr
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.