Dear editors,
We are aware that donors tobacco smoking history is quite common in the lung donor pool and several studies have investigated this aspect in order to understand whether this habit may influence the outcomes of recipients transplanted with lungs from smoking-donors (1,2). At the same time, there is very little literature focusing on donors’ marijuana smoking history as a factor affecting lung transplant (LTx) outcomes with conflicting results on early and intermediate (3,4) lung transplant outcomes.
We would like to focus the attention of the clinicians involved in LTx on a case of a 50 years-old patient, affected by idiopathic pulmonary fibrosis in therapy with nintedanib, who underwent bilateral lung transplantation at our Unit.
The donor was a 21 year-old male patient, admitted to the Intensive Care Unit (ICU) for a traumatic brain hemorrhage, with an unremarkable medical history except for cannabis abuse. Oto Score was 0 and all microbiological tests were negative.
The lung transplantation was performed with the usual surgical technique and peri and post-operative antibacterial prophylaxis was performed with combined antibiotics.
Antifungal and Cytomegalovirus prophylaxis and immunosuppressive therapy were based on aerosolized amphotericin B, ganciclovir and corticosteroids, mycophenolate mofetil, and cyclosporine respectively.
During the post-surgical phase, one blood culture was positive for Staphilococcus Epidermidis and two bronchial aspirates were positive for Acinetobacter baumannii and Klebsiella pneumonia, respectively.
Since the clinical conditions of the recipient were progressively improving, he was considered ready to be discharged. Before discharge, he underwent a bronchoscopy to perform surveillance trans-bronchial biopsies. The sample was insufficient. The histological examination showed diffuse alveolar damage and organizing pneumonia, as signs of ischemia reperfusion injury, while neither acute cellular rejection/lymphocytic bronchiolitis, infection, or marijuana-related lesions were detected.
The day after the procedure, the recipient presented a massive hemoptysis with cardiac arrest that required re-intubation and re-admission to the ICU. Since then, numerous episodes of hemoptysis have occurred and the patient died 10 days later because of hypovolemic shock.
A CT scan, performed the day before the exitus, showed multiple bilateral nodules which have been due to the hemorrhagic episodes and a small wedge-shaped cavitated lesion (arrow) could suggest, ex post, a possible aspergillosis (Supplementary Figure 1). An autopsy was then performed and histological examination of the lungs revealed an invasive pulmonary aspergillosis (IPA) (Figure 1) and smoking-related lesions (chronic bronchiolitis/bronchitis with infiltration of heavily pigmented macrophages) in the few evaluable areas. A timeline describing all the events is represented in Supplementary Figure 2.
FIGURE 1
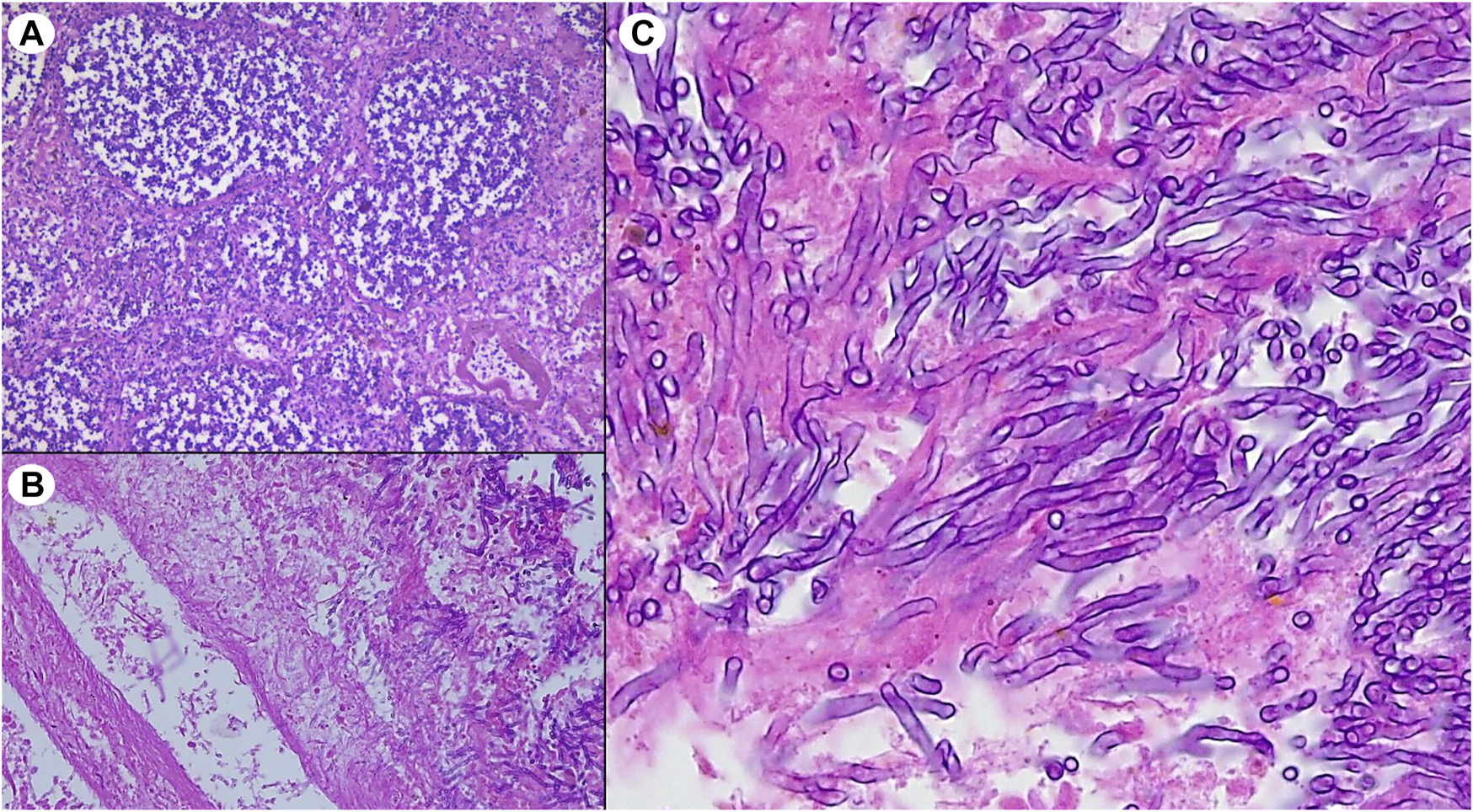
Histological lung sections from recipient’s autopsy showing (A) multiple foci of bronchopneumonia, (B) vascular erosion associated with widespread blood extravasation and, (C) well recognizable fungal branched hyphae compatible with Aspergillus spp.
A correlation between inhalation of marijuana and IPA has already been reported in renal (5) and bone marrow recipients (6) but, to the best of our knowledge, this is the first report of fatal early onset IPA in a patient who received lungs from a donor with ongoing marijuana use. We believe that, in our patient, a correlation between the donor’s marijuana smoking history and IPA could be supposed since no other explanation justified the development of such clinical picture.
However, it must be taken into account that such a clinical manifestation is anecdotal also considering the increasing prevalence of cannabis use between 2010 and 2019 in Europe (+27% in the population between 15 and 64 years) (7).
Despite this, since organ donors are often included in this age group, we would like to raise awarness in clinicians suggesting an accurate evaluation of the lungs retrieved from donors with ongoing marijuana abuse.
In case of young donors with cannabis smoking history, the pre-emptive research of fungi (especially Aspergillus) on biological samples should always be encouraged. At the same time, more sensitive tools, like polymerase chain reactions, could help in the early detection of Aspergillus in recipients with bleeding unrelated to the surgical procedure undergone.
Statements
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Author contributions
EF and FP designed the research and wrote the paper. AD’A, FL, CG, MM, MS, AC, and ML collected the data. FC and FR revised the paper.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontierspartnerships.org/articles/10.3389/ti.2022.10070/full#supplementary-material
Supplementary Figure 1CT scan iperformed the day before the exitus
Supplementary Figure 2timeline with representation of the events
Abbreviations
ICU, intensive care unit; IPA, invasive pulmonary aspergillosis; LTx, lung transplantation
References
1.
Schiavon M Lloret Madrid A Lunardi F Faccioli E Lorenzoni G Comacchio GM et al Short- and Long-Term Impact of Smoking Donors in Lung Transplantation: Clinical and Pathological Analysis. Jcm (2021). 10:2400. 10.3390/jcm10112400
2.
Oto T Griffiths AP Levvey B Pilcher DV Whitford H Kotsimbos TC et al A Donor History of Smoking Affects Early but Not Late Outcome in Lung Transplantation. Transplantation (2004). 78:599–606. 10.1097/01.tp.0000131975.98323.13
3.
Okahara S Levvey B McDonald M D'Costa R Opdam H Pilcher DV et al Influence of the Donor History of Tobacco and Marijuana Smoking on Early and Intermediate Lung Transplant Outcomes. J Heart Lung Transplant (2020). 39:962–9. 10.1016/j.healun.2020.05.019
4.
Mohite PN Zeriouh M Sáez DG Popov A-F Sabashnikov A Zych B et al Influence of History of Cannabis Smoking in Selected Donors on the Outcomes of Lung Transplantation. Eur J Cardiothorac Surg (2017). 51:142–7. 10.1093/ejcts/ezw255
5.
Marks WH Florence L Lieberman J Chapman P Howard D Roberts P et al Successfully Treated Invasive Pulmonary Aspergillosis Associated with Smoking Marijuana in a Renal Transplant Recipient. Transplantation (1996). 61:1771–4. 10.1097/00007890-199606270-00018
6.
Hamadeh R Ardehali A Locksley RM York MK . Fatal Aspergillosis Associated with Smoking Contaminated Marijuana, in A Marrow Transplant Recipient. Chest (1988). 94:432–3. 10.1378/chest.94.2.432
7.
Manathey J Freeman TP Kilian K Lopez-Pelayo H Rehm J . Public Health Monitoring of Cannabis Use in Europe: Prevalence of Use, Cannabis Potency, and Treatment Rates. The Lancet Reg Health- Europe (2021). 10:100227. 10.1016/j.lanepe.2021.100227
Summary
Keywords
lung transplantation, Aspergillosis, marijuana-smoking donor, infection, fatal outcome
Citation
Faccioli E, Pezzuto F, Dell’Amore A, Lunardi F, Giraudo C, Mammana M, Schiavon M, Cirnelli A, Loy M, Calabrese F and Rea F (2022) Fatal Early-Onset Aspergillosis in a Recipient Receiving Lungs From a Marijuana-Smoking Donor: A Word of Caution. Transpl Int 35:10070. doi: 10.3389/ti.2022.10070
Received
29 September 2021
Accepted
11 January 2022
Published
14 February 2022
Volume
35 - 2022
Updates
Copyright
© 2022 Faccioli, Pezzuto, Dell’Amore, Lunardi, Giraudo, Mammana, Schiavon, Cirnelli, Loy, Calabrese and Rea.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eleonora Faccioli, faccioli.eleonora@gmail.com, eleonora.faccioli@unipd.it
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.