Abstract
Scrub typhus (ST), also known as tsutsugamushi disease, is a rickettsial disease caused by Orientia tsutsugamushi. ST is widely endemic in Asia, including in Japan. ST can be fatal if the diagnosis is delayed. It has been reported that most fatal cases in northeastern Japan occur in spring and summer. We report an 80-year-old Japanese female case of ST who presented with fever and dyspnea without rash. Upon hospitalization, she was diagnosed with pneumonia with disseminated intravascular coagulation (DIC). Although an eschar was found on her lumbar region, she died from sepsis. Elevated tsutsugamushi antibody of IgM (Karp: 1:2560 dilution) was revealed. The diagnosis of ST was made postmortem. We reviewed 11 patients with ST at our hospital in northeastern Japan. All cases occurred in spring or summer and all showed the Karp strain. The prevalence of DIC was 64% and the mortality was 9.1%. We speculate that the Karp serotype may be prone to DIC, which may result in deteriorated condition. Two cases (18.2%), including the present case, showed no rash. The diagnosis of fatal ST may be difficult because it presents less frequently with rash and because it is accompanied by various complications such as pneumonia. When we see a patient with DIC of unknown cause in northeastern Japan in spring or summer, we should keep ST in mind, even if there is no skin rash.
Introduction
Scrub typhus (ST), also known as tsutsugamushi disease, is a rickettsial disease caused by the mite-borne bacterium Orientia tsutsugamushi (O. tsutsugamushi) [1]. When the bacterium is transmitted to a human, it begins to multiply at the bite site, where a black crust called an eschar forms. The rickettsia then spreads systemically, causing various symptoms, such as fever, rash, and lymphadenopathy [2–4]. Although some specific antibiotics, including tetracycline, azithromycin, and rifampicin, are effective against ST [5], the disease can be fatal if the diagnosis is delayed, and serious complications can occur, such as disseminated intravascular coagulation (DIC) [4, 6].
Here, we present a case of ST in northeastern Japan that had no rash and that was fatal due to DIC. ST cases at our hospital were accumulated, and a retrospective study was conducted to determine the prevalence of DIC in ST cases and to investigate the factors associated with DIC in such cases.
Case description
An 80-year-old Japanese woman presented with an 11-day history of fever and dyspnea. At the initial examination, her body temperature was 38.2°C, heart rate 96/min, blood pressure 118/53 mmHg, respiratory rate 24/min, and SpO2 99% (oxygen 4 L/min). There were no skin rashes on her body. Laboratory tests revealed elevated C-reactive protein (12.0 mg/dL), coagulation disorder (platelets 16 × 109/L, FDP 40.4 μg/mL) and liver failure (AST 123 IU/L, ALT 106 IU/L, LDH 676 IU/L, γ-GTP 81 IU/L). According to the Japanese Association for Acute Medicine (JAAM) DIC criteria, her total DIC score was 7, which met the diagnostic criteria for DIC [7]. In addition to these abnormal laboratory findings and symptoms, a chest X-ray showed permeability reduction (Figure 1); thus, she was diagnosed with pneumonia with DIC. Although ampicillin/sulbactam was initiated, her condition worsened. On day 4 after administration, an eschar was found on her lumbar region (Figure 2) and ST was suspected. The ampicillin/sulbactam was changed to minocycline. However, she died a few hours later from sepsis. Elevated tsutsugamushi antibody of IgM (Karp: 1:2560 dilution) was revealed afterwards; thus, the diagnosis of ST was confirmed postmortem.
FIGURE 1
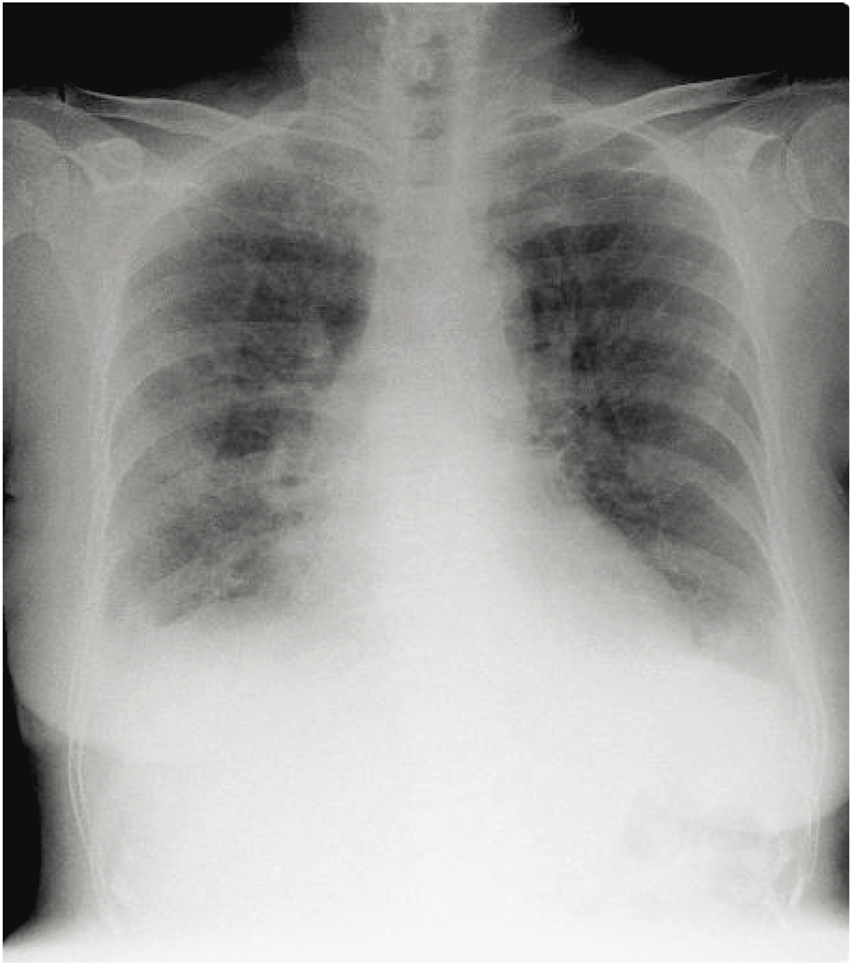
A chest X-ray at the initial examination shows permeability reduction.
FIGURE 2

An eschar appears on the lumbar region as an erythematous ulceration of about 10 mm in diameter covered with a black crust.
Discussion
Fever, rash, and eschar are the characteristic triad of ST [2, 3, 8]. In addition to these specific manifestations, liver failure, renal failure, interstitial pneumonia, meningitis/encephalitis, and DIC have been reported as complications [2–4, 9]. DIC is reported to be associated with more severe ST [9]. Moreover, DIC has been reported to be more prevalent in ST patients in northeastern Japan (28%) than in Japan overall (14%) [3].
To determine the prevalence of DIC in ST cases and to investigate the factors associated with DIC in such cases in northeastern Japan, we conducted a review of patients with ST at Noshiro Kousei Medical Center, in northeastern Japan, between 2010 and 2022 (Table 1). This study was approved by the internal review board of Noshiro Kousei Medical Center (YH-081). The review found 15 patients with ST; however, 4 of these patients were excluded because the data were insufficient for determining whether the criteria for DIC were met. Of the remaining 11 patients, 5 were men, and the median age of the 11 patients was 70 years (range 56–80 years). The patients had all been diagnosed with ST in spring or summer. The JAAM DIC criteria at the initial examination were adapted. These criteria consist of the following variables: systemic inflammatory response syndrome criteria (≥3: 1 point), platelet count (×109/L) (≥80 and <120, or >30% decrease within 24 h: 1 point; <80 or >50% decrease within 24 h: 3 points), prothrombin time ratio (≥1.2: 1 point), FDP (µg/mL) (≥10 but <25: 1 point; ≥25: 3 points). Scores of 4 or greater indicate a diagnosis of DIC [7]. Seven patients (64%) had ST accompanied by DIC. Of these, only the present case died of DIC secondary to ST (mortality 9.1%). Although all patients showed fever and eschar, skin rash was absent in two cases, including the present case. Regarding serotype, the Karp strain was identified in all patients.
TABLE 1
| Case | Age/Sex | Onset | Clinical symptoms | DIC | Hospitalization | Serotype | Outcome | ||
|---|---|---|---|---|---|---|---|---|---|
| Rash | Eschar | Fever | |||||||
| 1 | 69/F | May | + | + | + | - | + | Karp | Alive |
| 2 | 68/M | May | + | + | + | + | + | Karp | Alive |
| 3 | 70/M | May | + | + | + | + | + | Karp | Alive |
| 4 | 75/F | April | - | + | + | - | - | Karp | Alive |
| 5 | 63/M | April | + | + | + | - | - | Karp | Alive |
| 6 | 56/M | April | + | + | + | - | - | Karp | Alive |
| 7 | 71/F | April | + | + | + | + | + | Karp | Alive |
| 8 | 60/F | July | + | + | + | + | + | Karp | Alive |
| 9 | 74/F | May | + | + | + | + | + | Karp | Alive |
| 10 | 73/M | May | + | + | + | + | + | Karp | Alive |
| 11 (Present case) | 80/F | May | - | + | + | + | + | Karp | Dead |
Clinical characteristics of the 11 cases of scrub typhus.
DIC, disseminated intravascular coagulation.
ST is widespread in Asia, including in Japan [2–4]. It is found in almost all regions of Japan, except in Hokkaido, Japan’s northernmost island [2]. Six O. tsutsugamushi serotypes have been found in Japan: three major serotypes (Karp, Gilliam and Kato), and three minor serotypes (Irie/Kawasaki, Hirano/Kuroki, and Shimokoshi) [8, 10, 11]. In Japan, the majority of patients with ST (73%) are over 60 years old [2]. ST occurrence by month of onset is bimodal in Japan; a large peak occurs in autumn/winter (78%), and a small peak occurs in spring/summer (22%). In northeastern Japan, however, ST tends to occur in spring or summer [2]. This is because the vector, the Leptotrombium pallidum (L. pallidum) mite, is cold-resistant and, in northern Japan, overwinters to become a vector in spring and summer. Consequently, the number of patients with ST in northeastern Japan is higher in spring/summer than in fall/winter [2, 3]. Furthermore, spring/summer ST cases in northeastern Japan have been reported to show more severe symptoms and higher mortality rates than ST cases in southern Japan [2, 3]. L. pallidum carries the Karp and Gilliam serotypes, which are intermediately or highly virulent [12]. Most ST cases are seniors, and fatal ST cases are older than non-fatal ST cases [2]. The most common activity associated with ST infection is farm work, followed by forestry and wild vegetable gathering [3]. The present case involved wild vegetable gathering in spring. Northeastern Japan is the one of the coldest and snowiest parts of Japan. Hence, seniors there tend to be less active in winter and more active in spring and summer. This is likely why the prevalence and mortality rate of ST in spring/summer is higher in northeastern Japan than in other areas of Japan. In fact, the present fatal case occurred in May, late spring.
The prevalence of DIC in ST cases is higher in northeastern Japan than in Japan overall [3]. At our hospital in northeastern Japan, the rate of ST cases with DIC was not only higher than the rate for Japan overall, but was also higher than the rate for northeastern Japan overall. Furthermore, all patients with ST at our hospital showed the Karp strain. These findings suggest that ST patients with the Karp strain might be more prone to DIC. Consequently, the mortality rate in northeastern Japan in spring/summer might be high.
Although we only reviewed patients with sufficient data to evaluate DIC, the patients who were excluded from this study can be regarded as not having been suspected of having DIC clinically. Even if these excluded patients are included, the prevalence of DIC at our hospital would be about 50%, which is still much higher than Japan overall [3].
The present case was accompanied by pneumonia without skin rash; thus, it took 4 days after admission to diagnose it as ST. It has been reported that the main clinical symptoms of ST, including the triad of fever, eschar and skin rash, are less frequent in fatal ST cases [2]. Furthermore, severe symptoms such as pneumonia and encephalitis are most prevalent in fatal ST cases than in non-fatal ST cases [2]. Therefore, the diagnostic delay due to the lack of specific symptoms and the severe complications could have been factors in the fatal outcome.
Although a high rate of DIC accompanying ST has been reported in northeastern Japan, the present study suggests that the rate may be even higher than reported. Furthermore, we speculate that ST patients with the Karp strain, which is prevalent in northeastern Japan, might be prone to DIC. Therefore, when we see a patient with DIC of unknown cause in northeastern Japan in spring or summer, we should keep ST in mind, even if there is no skin rash. Also, ST patients with the Karp strain should be monitored for signs of DIC.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Noshiro Kousei Medical Center (YH-081). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because participants are included in this research using an opt out approach.
Author contributions
HS and NE contributed to the conception and design of the study, analysis of data, drafting of the manuscript. MK contributed to critical manuscript revision and final approval. YA and HY contributed to the acquisition of data and investigation. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
References
1.
Tamura A Ohashi N Urakami H Miyamura S . Classification of Rickettsia tsutsugamushi in a new genus, Orientia gen. nov., as Orientia tsutsugamushi comb. nov. Int J Syst Bacteriol (1995) 45(3):589–91. 10.1099/00207713-45-3-589
2.
Kinoshita H Arima Y Shigematsu M Sunagawa T Saijo M Oishi K et al Descriptive epidemiology of rickettsial infections in Japan: scrub typhus and Japanese spotted fever, 2007-2016. Int J Infect Dis (2021) 105:560–6. 10.1016/j.ijid.2021.02.069
3.
Ogawa M Hagiwara T Kishimoto T Shiga S Yoshida Y Furuya Y et al Scrub typhus in Japan: epidemiology and clinical features of cases reported in 1998. Am J Trop Med Hyg (2002) 67(2):162–5. 10.4269/ajtmh.2002.67.162
4.
Xu G Walker DH Jupiter D Melby PC Arcari CM . A review of the global epidemiology of scrub typhus. Plos Negl Trop Dis (2017) 11(11):e0006062. 10.1371/journal.pntd.0006062
5.
El SI Liu Q Wee I Hine P . Antibiotics for treating scrub typhus. Cochrane Database Syst Rev (2018) 9(9):CD002150. 10.1002/14651858.CD002150.pub2
6.
Ono Y Ikegami Y Tasaki K Abe M Tase C . Case of scrub typhus complicated by severe disseminated intravascular coagulation and death. Emerg Med Australas (2012) 24(5):577–80. 10.1111/j.1742-6723.2012.01600.x
7.
Gando S Iba T Eguchi Y Ohtomo Y Okamoto K Koseki K et al A multicenter, prospective validation of disseminated intravascular coagulation diagnostic criteria for critically ill patients: comparing current criteria. Crit Care Med (2006) 34(3):625–31. 10.1097/01.ccm.0000202209.42491.38
8.
Sando E Suzuki M Katoh S Fujita H Taira M Yaegashi M et al Distinguishing Japanese spotted fever and scrub typhus, Central Japan, 2004-2015. Emerg Infect Dis (2018) 24(9):1633–41. 10.3201/eid2409.171436
9.
Lee HJ Park CY Park SG Yoon NR Kim DM Chung CH . Activation of the coagulation cascade in patients with scrub typhus. Diagn Microbiol Infect Dis (2017) 89(1):1–6. 10.1016/j.diagmicrobio.2017.06.011
10.
Niid MHLW . Scrub typhus and Japanese spotted fever in Japan 2007-2016. Infect Agents Surveil Rep (2017) 38:109–12. Available online at: https://www.niid.go.jp/niid/en/iasr-vol38-e/865-iasr/7342-448te.html (Accessed July 22, 2024).
11.
Ohashi N Koyama Y Urakami H Fukuhara M Tamura A Kawamori F et al Demonstration of antigenic and genotypic variation in Orientia tsutsugamushi which were isolated in Japan, and their classification into type and subtype. Microbiol Immunol (1996) 40(9):627–38. 10.1111/j.1348-0421.1996.tb01120.x
12.
Nagano I Kasuya S Noda N Yamashita T . Virulence in mice of Orientia tsutsugamushi isolated from patients in a new endemic area in Japan. Microbiol Immunol (1996) 40(10):743–7. 10.1111/j.1348-0421.1996.tb01135.x
Summary
Keywords
disseminated intravascular coagulation, Karp strain, Orientia tsutsugamushi , rickettsia, scrub typhus, serotype
Citation
Sato H, Enzan N, Akasaka Y, Yajima H and Kono M (2025) Case Report: The relation between the incidence of disseminated intravascular coagulation in scrub typhus cases and its serotype in northeastern Japan. J. Cutan. Immunol. Allergy 8:14673. doi: 10.3389/jcia.2025.14673
Received
25 March 2025
Accepted
16 April 2025
Published
28 April 2025
Volume
8 - 2025
Updates
Copyright
© 2025 Sato, Enzan, Akasaka, Yajima and Kono.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Naoko Enzan, enzan0403@yahoo.co.jp; Michihiro Kono, miro@med.akita-u.ac.jp
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.