Abstract
Background:
The utilization of the robotic platform for ventral hernia repair is increasing, however is facing criticism for perceived high costs. This study aimed to compare the procedure-specific costs of robot-assisted ventral or incisional hernia repair with laparoscopic repair.
Methods:
This propensity score-matched nationwide database study included patients undergoing primary ventral and incisional hernia repair from 2017 to 2022. A total of 554 patients undergoing robot-assisted repair were matched 1:1 with patients undergoing laparoscopic repair by the confounding variables of age, type of hernia (primary ventral/incisional), and horizontal defect size. The primary outcome was the total cost per procedure in Euros including robotic/laparoscopic approach, mesh, tackers, length of stay, readmission, and operative reintervention. The price of obtaining laparoscopic and robotic systems was not included.
Results:
The length of stay was significantly shorter, and readmission rate was significantly lower for robot-assisted repairs (0.5 days and 7.0%) than for laparoscopic repairs (1.2 days and 12.5%), P < 0.001 and P = 0.003, respectively. The mean procedural cost of an incisional hernia repair was significantly reduced with the robot-assisted approach (1,533 Euros (sd: 1,584)) compared to the laparoscopic approach (2,077 Euros (sd: 1,840), P = 0.002). Multivariable linear regression analysis confirmed that robotic ventral hernia repair was independently associated with decreased overall costs (coeff −682.1, CI −1,331.5 - −32.6, P = 0.040).
Conclusion:
For primary ventral hernias, the mean procedural costs of a robot-assisted and a laparoscopic repair are comparable, but for incisional hernia repairs the mean procedural cost is decreased with a robot-assisted approach.
Introduction
Primary ventral and incisional hernia repairs are common elective procedures that can be done through either open or minimally invasive methods. Open repairs have a notable risk of wound-related complications, which can lead to higher short-term patient morbidity, increased hospital costs, and a greater long-term risk of hernia recurrence [1–3].
Laparoscopic ventral hernia repair was introduced three decades ago and proved to be superior to open repair in terms of decreasing wound complications and suggestively even reducing recurrence rates [4–8]. Laparoscopic ventral hernia repair is conventionally performed as an IPOM (intraperitoneal onlay mesh) technique, where an intraperitoneal mesh is fixated to the abdominal wall with tackers and/or transfascial sutures [9]. Overall, the IPOM approach has good long-term results, but rare, severe complications, such as intestinal adhesions to the intraperitoneal mesh, as well as acute and chronic pain due to traumatic mesh fixation may occur [7]. Meanwhile, the increased access to the robotic platform in high income countries has facilitated the spread of more technically advanced minimally invasive procedures with mesh placement outside the peritoneal cavity avoiding traumatic fixation [10, 11].
Compared to open approaches robot-assisted ventral hernia repair has proven to be superior in terms of less postoperative pain, faster recovery, and fewer wound complications [12–16]. As the robotic platform makes it easier to avoid intraperitoneal mesh and the use of tacks for fixation, there is less postoperative pain, shorter length of stay, and lower risk of readmission compared to laparoscopic IPOM [17–19]. Nonetheless, opponents of the robotic approach argue that it is too costly with prolonged operating times and insufficient data to demonstrate improved patient-related outcomes [20, 21]. Conversely, coated meshes for intraperitoneal use and tacker devices for laparoscopic ventral hernia are also expensive. Thus, if length of stay and readmission rate increase, the costs of a laparoscopic approach may surpass that of a robot-assisted approach.
The hypothesis of the present study was that the procedural costs of robot-assisted primary ventral or incisional hernia repair are equal to or lower compared to laparoscopic repair due to shorter length of stay, lower risk of readmission, and less expensive materials. The aim of this study was to compare the procedure-specific costs of a robot-assisted ventral or incisional hernia repair to a laparoscopic repair, including expenses related to readmissions and reoperations within 90 days postoperatively.
Methods
Patient Cohort
Since 2007, all hernia repair patients in Denmark have been registered in the Danish Hernia Database without patient consent. Surgeons record details such as hernia type, defect size, mesh type, and fixation method. In 2017, smoking and BMI data were added. The National Patients Registry logs all patient interactions with the healthcare system, including Charlson Comorbidity Index scores, hospital stay duration, readmissions, and reoperations within 90 days. Data for this study were obtained by merging these two databases using each patient’s unique identification number [22]. Patients were included from Jan 1st 2017 to December 31st 2022. Patients undergoing elective primary ventral or incisional hernia repair by either robot-assisted or laparoscopic approach were included. Converted procedures were not included.
Cost Analysis
The study’s primary outcome was the total mean cost per procedure in Euros. A cost analysis compared laparoscopic and robot-assisted procedures, assuming similar staff numbers and comparable anesthesia and basic instrument costs. The cost variables included were: robot-assisted approach, laparoscopic approach, extra ports (if more than three used), mesh, tackers, hospital stay length, readmission, and surgical reintervention.
The cost of a robot-assisted procedure included the instrument arm drape, three instrument cannulas, obturators, cannula seal, tip covers, and instruments such as monopolar curved scissors, fenestrated bipolar forceps, and a mega suture cut needle driver. The cost of a laparoscopic procedure included ports, scissors or energy devices, and a smoke evacuation tube (Supplementary Table). The costs for buying and maintaining the laparoscopic and robotic systems were not included.
The daily cost for postoperative hospital stay and readmissions within 90 days was calculated using the national Diagnosis Related Grouping (DRG) rate, which measures hospital costs associated with procedures. The same system was used to estimate the cost of reoperation, applying the DRG rate “Other operations and treatments on digestive organs without complicated secondary diagnoses” to avoid overestimation. The same price was applied for every surgical reintervention.
Statistics
To reduce heterogeneity, robot-assisted primary ventral and incisional hernia repairs were propensity-score matched in a 1:1 ratio with patients undergoing laparoscopic repair. Patients were matched by age, type of hernia (primary ventral/incisional), and horizontal defect size using nearest neighbor matching with a caliper of 0.05. Numerical variables were reported as mean (standard deviation, SD) or median (range) and compared across the two groups using Student’s t-test or Mann–Whitney U test where appropriate. Categorical variables were reported as n (%) and compared across groups using the Chi-squared test. A multiple linear regression analysis was performed to examine the association between mean total cost per procedure and the confounding variables. Additionally, a subgroup analysis of patients undergoing either primary or incisional hernia repair was conducted to evaluate the costs for the specific hernia types.
P-values <0.05 were considered statistically significant. The data analysis was performed using R software version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
This study was approved by the Danish Data Protection Agency (ref. P-2021-58). A protocol was made before study start but was not published online. The study was registered at ClinicalTrials.gov identifier: NCT06232148. The study is reported according to the STROBE reporting guidelines for observational studies [23].
Results
A total of 554 patients undergoing robot-assisted primary ventral or incisional hernia repair were matched with 554 patients undergoing laparoscopic repair (Figure 1; Table 1). A total of 35.7% (198/554) of the patients underwent incisional hernia repair and 73.5% (407/554) had a defect width <4 cm. There were no significant differences between the two groups regarding age, sex, smoking status, BMI, and Charlson Comorbidity Index score (Table 1).
FIGURE 1
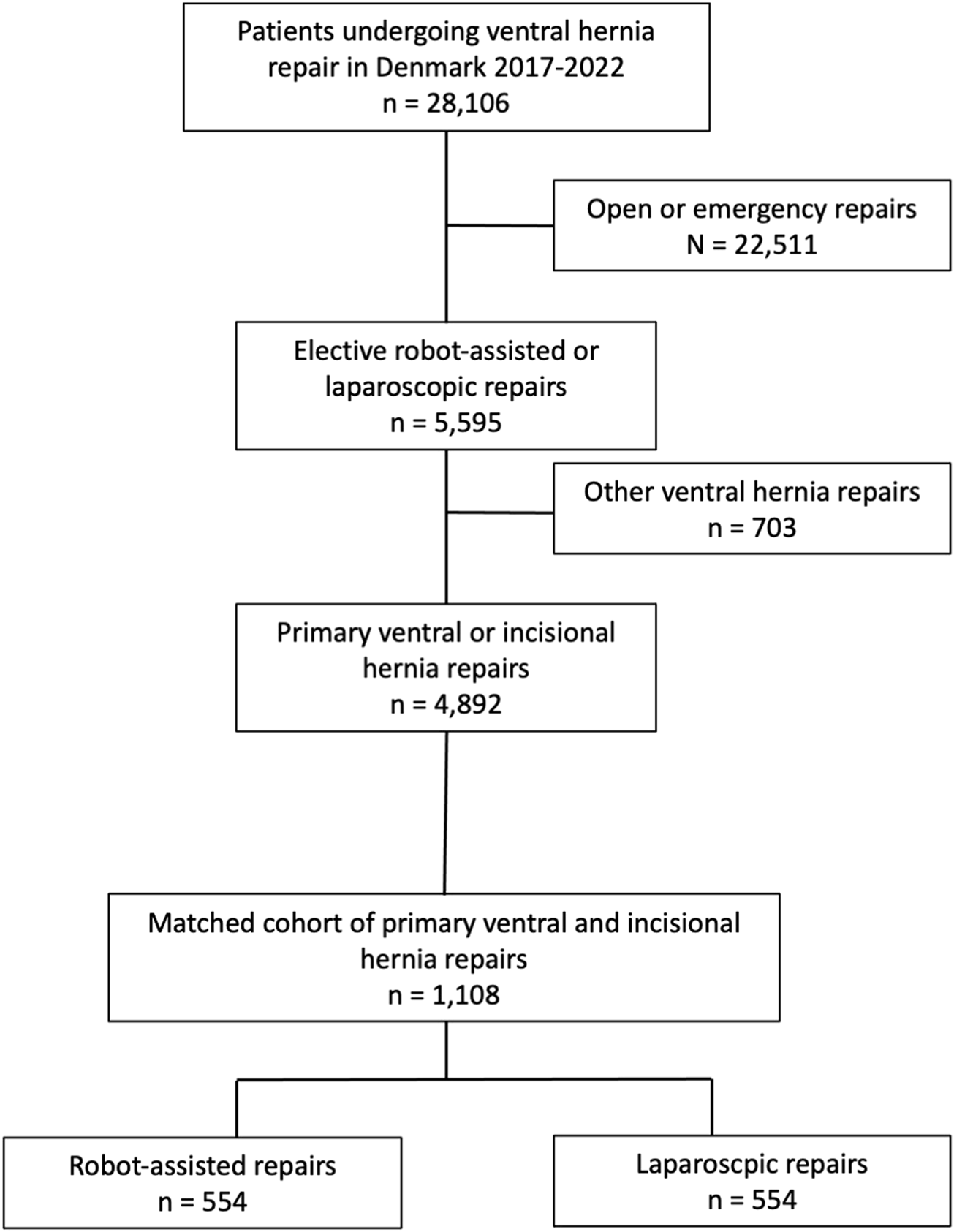
Flowchart of patient inclusion.
TABLE 1
| Variables | Robot-assisted repair (n = 554) | Laparoscopic repair (n = 554) | P | |
|---|---|---|---|---|
| Age (years) | <45 | 93 (16.8) | 117 (21.1) | 0.236 |
| 45–60 | 196 (35.4) | 198 (35.7) | ||
| >60–75 | 216 (39.0) | 198 (35.7) | ||
| >75 | 49 (8.8) | 41 (7.4) | ||
| Sex | female | 239 (43.1) | 249 (44.9) | 0.586 |
| Smoking | Yes | 91 (16.4) | 69 (12.5) | 0.073 |
| Charlson Comorbidity Index | 0 | 307 (55.4) | 305 (55.1) | 0.430 |
| 1 | 92 (16.6) | 79 (14.3) | ||
| >1 | 155 (28.0) | 170 (30.7) | ||
| BMI (kg/m2) | mean [range] | 30.2 [19.7, 50.8] | 30.3 [12.5, 51.6] | 0.769 |
| missing | 257 | 182 | ||
| categorized (kg/m2) | <30 | 158 (53.2) | 192 (51.6) | 0.450 |
| 30–35 | 89 (30.0) | 75 (20.2) | ||
| >35 | 50 (16.8) | 105 (28.2) | ||
| Type of hernia | Primary ventral | 356 (64.3) | 356 (64.3) | 100 |
| Incisional | 198 (35.7) | 198 (35.7) | ||
| Vertical defect size (cm) | mean (sd) | 4.5 (5.1) | 3.9 (5) | 0.064 |
| Horizontal defect size (cm) | mean (sd) | 4 (4.6) | 3.6 (4.7) | 0.238 |
| categorized (cm) | <4 | 407 (73.5) | 407 (73.5) | 100.000 |
| 4–8 | 127 (22.9) | 127 (22.9) | ||
| >8 | 20 (3.6) | 20 (3.6) | ||
| Year of surgery | 2017 | 30 (5.4) | 204 (36.8) | <0.001 |
| 2018 | 88 (15.9) | 156 (28.2) | ||
| 2019 | 108 (19.5) | 61 (11.0) | ||
| 2020 | 102 (18.4) | 66 (11.9) | ||
| 2021 | 146 (26.4) | 33 (6.0) | ||
| 2022 | 80 (14.4) | 34 (6.1) | ||
| Mesh position | Preperitoneal | 109 (19.7) | 128 (23.1) | <0.001 |
| Retromuscular | 419 (75.6) | 0 (0.0) | ||
| Intraperitoneal | 26 (4.7) | 426 (76.9) | ||
| Mesh fixation method | Glue and tackers/clips | 5 (0.9) | 0 (0.0) | <0.001 |
| Glue | 22 (4.0) | 4 (0.7) | ||
| Self fixating mesh | 377 (68.1) | 12 (2.2) | ||
| Tackers | 8 (1.4) | 373 (67.3) | ||
| Glue and suture | 4 (0.7) | 0 (0.0) | ||
| Clips | 0 (0.0) | 3 (0.5) | ||
| Suture | 49 (8.8) | 69 (12.5) | ||
| Tackers and suture | 9 (1.6) | 78 (14.1) | ||
| None | 76 (13.7) | 11 (2.0) | ||
| Other | 4 (0.7) | 4 (0.7) | ||
| Defect closure | Yes | 538 (97.1) | 406 (73.3) | <0.001 |
| Length of stay (days) | mean [range] | 0.5 [0, 32] | 1.2 [0, 29] | <0.001 |
| missing | 22 | 15 | ||
| Readmission, n (%) | Yes | 39 (7.0) | 69 (12.5) | 0.003 |
| Reoperation, n (%) | Yes | 11 (2.0) | 21 (3.8) | 0.106 |
Demographics of patients undergoing robot-assisted and laparoscopic ventral and incisional hernia repair.
SD, Standard deviation; BMI, Body Mass Index.
In robot-assisted repairs, the mesh was most often placed in the retromuscular position 75.6% (419/554), and most frequently this was a self-fixating mesh 68.1% (337/554). For the laparoscopic repairs, the mesh was placed in the intraperitoneal position in 76.9% (426/554) and fixated with tackers in 67.3% (373/554) of the cases. In the robotic group, 4.9% (27/554) of the patients underwent a transversus abdominis release (TAR) as opposed to 0% in the laparoscopic group.
Length of stay was significantly shorter after a robot-assisted repair compared to a laparoscopic repair (mean 0.5 days vs. 1.2 days, P < 0.001). The readmission rate was significantly lower for robot-assisted repairs 7.0% (39/554) compared with laparoscopic repairs 12.5% (69/554), P = 0.003. There were no significant differences in the rate of surgical reintervention after robot-assisted or laparoscopic repair (2.0%, 11/554 vs. 3.8%, 21/554), P = 0.106 (Table 1).
The mean cost of basic equipment for a robot-assisted approach was significantly higher compared to laparoscopic approach (865.3 vs. 471.6 Euros, P < 0.001). The mean costs of mesh and tack devices were significantly higher in the laparoscopic group (415 Euros and 153 Euros) than in the robotic group (191 Euros and 10 Euros), P < 0.001, respectively. Mean costs of readmission and reoperation were not significantly higher in the laparoscopic group (425 Euros and 145 Euros) than in the robot-assisted group (63 Euros and 95 Euros), P = 0.257 and P = 0.277, respectively (Table 2). The mean total cost of all robot-assisted primary ventral and incisional hernia repairs was less after robotic compared to laparoscopic repair (1,326.2 vs. 1,990.1 Euros, P = 0.045). Multivariable linear regression analysis confirmed that robotic ventral hernia repair was independently associated with decreased overall costs (coeff −682.1, CI −1,331.5 - −32.6, P = 0.040, Table 3). In addition, defect size between 4 and 8 cm was associated with increased costs.
TABLE 2
| Variables | Robot-assisted repair (n = 554) | Laparoscopic repair (n = 554) | P | |
|---|---|---|---|---|
| Costs (Euros) | ||||
| Robotic approach | Mean (sd) | 865.3 (0) | 0 (0) | <0.001 |
| Laparoscopic approach | Mean (sd) | 0 (0) | 471.6 (0) | <0.001 |
| Mesh | Mean (sd) | 153 (86) | 415 (130) | <0.001 |
| Tackers | Mean [sd] | 10 (48) | 191 (91) | <0.001 |
| Length of stay | Mean (sd) | 140 (557) | 344 (677) | <0.001 |
| Readmission | Mean (sd) | 63 (365) | 425 (7,514) | 0.257 |
| Reoperation | Mean (sd) | 95 (730) | 145 (785) | 0.277 |
| Total | Mean (sd) | 1,326.2 (1,189.8) | 1,990.8 (7,720.8) | 0.045 |
Mean total cost per patient for robot-assisted and laparoscopic primary ventral and incisional hernia repair.
TABLE 3
| Variables | Coefficient | 95% CI | P | |
|---|---|---|---|---|
| Age (years) | 21.4 | [-4.95; 47.8] | 0.112 | |
| Sex | Female | Ref | ||
| Male | 267.0 | [-398.7; 932.7] | 0.432 | |
| Charlson Comorbidity Index | 0 | Ref | ||
| 1 | 68.2 | [-881.9; 1,018.3] | 0.888 | |
| >1 | 762.7 | [-51.1; 1,576.5] | 0.067 | |
| Horizontal defect, cm | <4 | Ref | ||
| 4–8 | 1,053.3 | [250.4; 1856.1] | 0.010 | |
| >8 | 362.8 | [-1,454.2; 2,179.9] | 0.696 | |
| Type of surgical approach | Laparoscopic | Ref | ||
| Robot-assisted | −682.1 | [-1,331.5;-32.6] | 0.040 | |
| Type of hernia | Incisional | Ref | ||
| Primary | 262.6 | [-488.5; 1,013.6] | 0.493 |
Multivariable analysis of factors associated with total costs for patients undergoing primary ventral or incisional hernia repair.
Primary Ventral and Incisional Hernia Repair Subgroup Analysis
A total of 712 patients in the study cohort underwent primary ventral hernia repair, either laparoscopic (n = 356) or robot-assisted (n = 356). Cost analysis of this subgroup found that the mean cost of robot-assisted repair was comparable to laparoscopic repair (1,211 Euros vs. 1,943 Euros, P = 0.149, Table 4). Multivariable linear regression analysis found no association of approach with the total costs of the procedure (robotic coeff −714.3, CI −1705.8 – 277.3, P = 0.158) for primary ventral hernia repair.
TABLE 4
| Variables | Robot-assisted repair (n = 356) | Laparoscopic repair (n = 356) | P | |
|---|---|---|---|---|
| Costs (Euros) | ||||
| Robotic approach | Mean (sd) | 865.3 (0) | 0 (0) | <0.001 |
| Laparoscopic approach | Mean (sd) | 0 (0) | 471.6 (0) | <0.001 |
| Mesh | Mean (sd) | 139 (54.6) | 395 (135.1) | <0.001 |
| Tackers | Mean [sd] | 7 (38.7) | 172 (103.6) | <0.001 |
| Length of stay | Mean (sd) | 92 (303.9) | 227 (558.7) | <0.001 |
| Readmission | Mean (sd) | 48 (330.5) | 551 (9,341.6) | 0.311 |
| Reoperation | Mean (sd) | 60 (552.2) | 127 (783.2) | 0.192 |
| Total | Mean (sd) | 1,210.7 (880.1) | 1,942.8 (9,537.9) | 0.149 |
Mean total cost per patient for robot-assisted and laparoscopic primary ventral hernia repair.
For the 396 patients undergoing incisional hernia repair (laparoscopic n = 198, robot-assisted n = 198), the mean cost per procedure was significantly lower after robot-assisted repair (1,534 Euros vs. 2,077 Euros, P = 0.002, Table 5). Multivariable linear regression analysis confirmed an independent significant association between surgical approach and total procedure-related costs (robotic coeff. −583.3, CI -922.1 - -244.6, P < 0.001) for incisional hernia repair.
TABLE 5
| Variables | Robot-assisted repair (n = 198) | Laparoscopic repair (n = 198) | P | |
|---|---|---|---|---|
| Costs (Euros) | ||||
| Robotic approach | Mean (sd) | 865.3 (0) | 0 (0) | <0.001 |
| Laparoscopic approach | Mean (sd) | 0 (0) | 471.6 (0) | <0.001 |
| Mesh | Mean (sd) | 178 (119.3) | 450 (112.5) | <0.001 |
| Tackers | Mean [sd] | 17 (60.1) | 225 (46.2) | <0.001 |
| Length of stay | Mean (sd) | 228 (832.9) | 555 (809.7) | <0.001 |
| Readmission | Mean (sd) | 88 (419) | 199 (1,071) | 0.177 |
| Reoperation | Mean (sd) | 158 (970) | 178 (789.2) | 0.826 |
| Total | Mean (sd) | 1,533.9 (1,584.4) | 2,077 (1,840.4) | 0.002 |
Mean total cost per patient for robot-assisted and laparoscopic incisional hernia repair.
Discussion
This nationwide database study compared the procedural costs of robot-assisted primary ventral or incisional hernia repairs with laparoscopic repairs and found the costs of a robot-assisted approach was less than traditional laparoscopic repair. In subgroup analysis, robot-assisted incisional hernia repair was found to be significantly less costly compared to laparoscopic repair, and multivariable analysis confirmed this association independently. Patients undergoing laparoscopic repair had more expensive meshes implanted, significantly longer hospital stay, and a higher rate of readmission, which added to the mean costs of the procedures. These findings suggest that a robot-assisted repair is associated with shorter hospitalization and fewer readmissions leading to a procedural cost that is less than that of a laparoscopic repair.
The result of the current study seems to confirm, that for robot-assisted hernia repair, the cost-effectiveness relies on the type of hernia. This may be because incisional hernia repair is technically more challenging compared to primary ventral hernia repair and thus a robotic approach to this patient group leads to improved outcomes. Further, the costs of the meshes used in either approach was significantly greater in laparoscopic repair, which most often was due to more expensive coated meshes placed intraperitoneal as compared to non-coated meshes placed preperitoneal or retromuscular in robot-assisted repairs. Placement of the mesh in the preperitoneal or retromuscular plane may be the technically more challenging and is easier facilitated by a robot-assisted approach. Placement of a non-coated mesh in the preperitoneal or retromuscular position is possible laparoscopically and would decrease the cost of the laparoscopic procedure, however, the data reflects that it is rarely done in Denmark, possibly because it is more difficult than an IPOM procedure or because of relatively high access to robotic platforms.
A nationwide analysis from the US found that robot-assisted ventral hernia repair was associated with shorter length of stay compared to both open and laparoscopic approach, but the hospital charges were significantly higher for the robotic approach [15]. Likewise, another study from the US concluded that hospital charges were 25% higher for a robot-assisted ventral hernia repair compared with a laparoscopic repair [24]. However, the reimbursement systems in Europe and US are very different and not directly comparable. A recent Brazilian study evaluated the direct costs associated with operating time, operating room personnel, and amount of medication, and it concluded that robot-assisted repairs were significantly more costly than laparoscopic repairs caused by longer operating room charges [25]. A multicenter randomized controlled trial concluded that the costs of robot-assisted and laparoscopic ventral hernia repairs were comparable; although the meshes in the laparoscopic group were more expensive, the increased operating time in the robotic group equalized the cost [26]. These differences in study outcomes illustrate the international variation and complexity of cost analyses.
Several studies conclude that the operating time is longer for robotic surgery, but a learning curve should be taken into account, and there is evidence that the operating time, as well as time for draping and docking of the robot, can be reduced significantly with increased experience [16, 27].
Interestingly, most studies investigating cost-effectiveness of the robotic platform solely focus on the direct procedure-related cost, and not on socioeconomical costs associated with readmissions, reoperations due to complications, or the costs associated with prolonged postoperative recovery such as sick leave or costs associated with obtaining assistance at home. As length of stay and risk of readmission was shorter in patients undergoing robot-assisted repair, these patients are probably more likely to return faster to work and daily activities, thereby reducing the overall societal and psychological expenses related to surgery.
The angulation of the robotic arms facilitates the minimally invasive approach to more complex repairs. In the current study we did not take the complexity of the hernia repair into account, but only matched patients on hernia type and horizontal defect size. Thus, although aiming for reducing the selection bias with propensity score matching, there may have been more complex repairs in the robotic group reflected by more performed TAR procedures than in the laparoscopic group, which would have further added to the benefit of the robotic repairs and decreased costs. Future studies are needed to clarify outcomes and cost-effectiveness of the robotic system in the largest and more complex ventral and incisional hernias.
This study is strengthened by its reliance on nationwide database data reflecting real world data with high external validity. However, there are limitations. The laparoscopic procedures performed were mainly IPOM procedures, whereas the robot-assisted procedures were various, and one may argue that these are not comparable. On the other hand, this is real-world data, and one of the advantages with the robotic system is easier placement of the mesh outside the peritoneal cavity. While this is also feasible laparoscopically, it is technically more challenging. Possibly, the laparoscopic procedures were performed by several different surgeons, and the robot-assisted surgeries were performed by a smaller group of hypothetically more experienced surgeons. On the other hand, the first robot-assisted procedures were included in this study, meaning that the study included cases in the early phase of the robotic learning curve, both factors could potentially have affected the results. The operative time is unfortunately not available from the Danish Hernia Database, which would have been relevant to include in the cost calculation. As robotic procedures, especially in the beginning of the learning curve, may take longer than laparoscopic procedures, calculation of cost associated to operative time could have affected the results.
Comprehensive cost calculations are difficult to perform and compare, as they vary across countries with different reimbursement systems, and inherently are based on the elements included in the computations. This cost calculation was based on the Danish system, which may not translate to other healthcare systems. A factor like length of stay may not be related to the procedure itself but to discharge traditions, patient-related factors and regional factors, as more laparoscopic repairs were performed in the early part of the study period, such factors could potentially have biased the results. In contrast, when a novel surgical procedure is implemented, such as robot-assisted ventral hernia repair, the surgeon may opt to keep the patient hospitalized for an additional day.
This cost analysis excluded expenses related to acquisition of the robotic platform and operating times, potentially underestimating the costs in the robotic group. Acquisition and maintenance costs may be attributed to different resources in the hospital (i.e., acquisition costs vs. daily expenses) and further, that the price of a robotic system may vary due to differences in hospital relations to the robotic system manufacturer or previous acquisitions in the hospital. Lastly, many hospitals already have a robotic system, but the system is not used for abdominal wall surgery, these findings suggest that if a system is present, it seems cost-effective to use it for ventral and incisional hernias [28]. Presumably, the price of acquiring a robot system is likely to change in the future, as more robotic systems are on the market and different agreements such as leasing or pay-per-procedure can be made with the companies. Furthermore, the study employed minimum prices for hospital stay, cost of readmissions and surgical reinterventions. Costs associated with further diagnostic work-up or interventions of readmitted patients, such as imaging diagnostics or epidural anesthesia, were not included in the cost calculation. Additionally, specific surgical equipment such as vacuum assisted closure (VAC), staplers or energy devices were not included in the cost of surgical reintervention, potentially impacting the overall costs.
In conclusion, while the costs of the robotic surgical equipment surpass that of conventional laparoscopy, it is offset by the need of more expensive meshes and tacker devices, and higher readmission rates following a laparoscopic approach. This nationwide database study showed that for primary ventral hernias, the mean procedural costs of a robot-assisted and a laparoscopic repair are comparable, but for incisional hernia repairs the mean procedural cost is decreased with a robot-assisted approach. Future cost analyses should be more comprehensive and include socioeconomic factors related to the postoperative phase to map the scope of robot-assisted hernia repair and its suggested benefits.
Statements
Data availability statement
The datasets presented in this article are not readily available because due to danish law, the dataset can’t be shared. Requests to access the datasets should be directed to nadiahenriksen@gmail.com.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
NH: Conceptualization, methodology, writing - original draft, review and editing. MW: Writing - original draft, review and editing. MM: Visualization, writing - review and editing. KJ: Conceptualization, methodology, formal analysis, writing - review and editing. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
NH has received speaker fees from Intuitive, Medtronic and Conmed. MW has received speaker fees from Intuitive and is Assistant Chief Editor in JAWS. KJ has received speaker fees from Bard, Conmed, Intuitive and Medtronic.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontierspartnerships.org/articles/10.3389/jaws.2025.15464/full#supplementary-material
References
1.
Badia JM Casey AL Petrosillo N Hudson PM Mitchell SA Crosby C . Impact of Surgical Site Infection on Healthcare Costs and Patient Outcomes: A Systematic Review in Six European Countries. J Hosp Infect (2017) 96:1–15. 10.1016/j.jhin.2017.03.004
2.
Holihan JL Alawadi Z Martindale RG Roth JS Wray CJ Ko TC et al Adverse Events After Ventral Hernia Repair: The Vicious Cycle of Complications. J Am Coll Surg (2015) 221:478–85. 10.1016/j.jamcollsurg.2015.04.026
3.
Cobb WS Warren JA Ewing JA Burnikel A Merchant M Carbonell AM . Open Retromuscular Mesh Repair of Complex Incisional Hernia: Predictors of Wound Events and Recurrence. J Am Coll Surg (2015) 220:606–13. 10.1016/j.jamcollsurg.2014.12.055
4.
Sauerland S Walgenbach M Habermalz B Seiler CM Miserez M . Laparoscopic Versus Open Surgical Techniques for Ventral or Incisional Hernia Repair. Cochrane Database Syst Rev CD007781 (2011) CD007781. 10.1002/14651858.CD007781.pub2
5.
Colavita PD Tsirline VB Walters AL Lincourt AE Belyansky I Heniford BT . Laparoscopic Versus Open Hernia Repair: Outcomes and Sociodemographic Utilization Results from the Nationwide Inpatient Sample. Surg Endosc (2013) 27:109–17. 10.1007/s00464-012-2432-z
6.
Henriksen NA Jorgensen LN Friis-Andersen H Helgstrand F , Danish Hernia Database. Open Versus Laparoscopic Umbilical and Epigastric Hernia Repair: Nationwide Data on Short- and Long-Term Outcomes. Surg Endosc (2022) 36:526–32. 10.1007/s00464-021-08312-5
7.
Henriksen NA Friis-Andersen H Jorgensen LN Helgstrand F . Open Versus Laparoscopic Incisional Hernia Repair: Nationwide Database Study. BJS Open (2021) 5(1):zraa010. 10.1093/bjsopen/zraa010
8.
Martins MR Santos-Sousa H do Vale MA Bouca-Machado R Barbosa E Sousa-Pinto B . Comparison Between the Open and the Laparoscopic Approach in the Primary Ventral Hernia Repair: A Systematic Review and Meta-Analysis. Langenbecks Arch Surg (2024) 409:52. 10.1007/s00423-024-03241-y
9.
LeBlanc KA Booth WV . Laparoscopic Repair of Incisional Abdominal Hernias Using Expanded Polytetrafluoroethylene: Preliminary Findings. Surg Laparosc Endosc (1993) 3:39–41.
10.
Muysoms F Van Cleven S Pletinckx P Ballecer C Ramaswamy A . Robotic Transabdominal Retromuscular Umbilical Prosthetic Hernia Repair (TARUP): Observational Study on the Operative Time During the Learning Curve. Hernia (2018) 22:1101–11. 10.1007/s10029-018-1825-x
11.
Anoldo P Manigrasso M D'Amore A Musella M De Palma GD Milone M . Abdominal Wall Hernias-State of the Art of Laparoscopic Versus Robotic Surgery. J Pers Med (2024) 14(1):100. 10.3390/jpm14010100
12.
Henriksen NA Jensen KK Muysoms F . Robot-Assisted Abdominal Wall Surgery: A Systematic Review of the Literature and Meta-Analysis. Hernia (2019) 23:17–27. 10.1007/s10029-018-1872-3
13.
Christoffersen MW Henriksen NA . Treatment of Primary Ventral and Incisional Hernias. Br J Surg (2023) 110:1419–21. 10.1093/bjs/znad137
14.
Dewulf M Hiekkaranta JM Makarainen E Saarnio J Vierstraete M Ohtonen P et al Open Versus Robotic-Assisted Laparoscopic Posterior Component Separation in Complex Abdominal Wall Repair. BJS Open (2022) 6(3):zrac057. 10.1093/bjsopen/zrac057
15.
Ayuso SA Katzen MM Aladegbami BG Nayak RB Augenstein VA Heniford BT et al Nationwide Readmissions Analysis of Minimally Invasive Versus Open Ventral Hernia Repair: A Retrospective Population-Based Study. Am Surg (2022) 88:463–70. 10.1177/00031348211050835
16.
Shenoy R Mederos MA Jacob RL Kondo KK DeVirgilio M Ward R et al Robot-Assisted General Surgery Procedures at the Veterans Health Administration: A Comparison of Surgical Techniques. J Surg Res (2022) 279:330–7. 10.1016/j.jss.2022.06.032
17.
Christoffersen MW Jorgensen LN Jensen KK . Less Postoperative Pain and Shorter Length of Stay After Robot-Assisted Retrorectus Hernia Repair (rRetrorectus) Compared with Laparoscopic Intraperitoneal Onlay Mesh Repair (IPOM) for Small or Medium-Sized Ventral Hernias. Surg Endosc (2022) 37:1053–9. 10.1007/s00464-022-09608-w
18.
Jensen KK Helgstrand F Henriksen NA . Short-Term Outcomes After Laparoscopic IPOM Versus Robot-Assisted Retromuscular Repair of Small to Medium Ventral Hernias: A Nationwide Database Study. Ann Surg (2023) 279:154–9. 10.1097/SLA.0000000000005915
19.
Bindal V Pandey D Gupta S . Laparoscopic Intra-Peritoneal Onlay Mesh Plus Versus Robotic Transabdominal Pre-Peritoneal for Primary Ventral Hernias: Our Technique and Outcomes. J Minim Access Surg (2024) 21:25–33. 10.4103/jmas.jmas_4_24
20.
Childers CP Maggard-Gibbons M . Estimation of the Acquisition and Operating Costs for Robotic Surgery. Jama (2018) 320:835–6. 10.1001/jama.2018.9219
21.
Ye L Childers CP de Virgilio M Shenoy R Mederos MA Mak SS et al Clinical Outcomes and Cost of Robotic Ventral Hernia Repair: Systematic Review. BJS Open (2021) 5(6):zrab098. 10.1093/bjsopen/zrab098
22.
Helgstrand F Jorgensen LN . The Danish Ventral Hernia Database - a Valuable Tool for Quality Assessment and Research. Clin Epidemiol (2016) 8:719–23. 10.2147/CLEP.S99501
23.
von Elm E Altman DG Egger M Pocock SJ Gotzsche PC Vandenbroucke JP et al The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. J Clin Epidemiol (2008) 61:344–9. 10.1016/j.jclinepi.2007.11.008
24.
Khorgami Z Li WT Jackson TN Howard CA Sclabas GM . The Cost of Robotics: An Analysis of the Added Costs of Robotic-Assisted Versus Laparoscopic Surgery Using the National Inpatient Sample. Surg Endosc (2019) 33:2217–21. 10.1007/s00464-018-6507-3
25.
Costa TN Tustumi F Ferros LSM Colonno BB Abdalla RZ Ribeiro-Junior U et al Robotic-Assisted Versus Laparoscopic Incisional Hernia Repair: Differences in Direct Costs from a Brazilian Public Institute Perspective. Arq Bras Cir Dig (2023) 35:e1714. 10.1590/0102-672020220002e1714
26.
Petro CC Montelione KC Zolin SJ Renton DB Yunis JP Meara MP et al Robotic Etep Versus IPOM Evaluation: The REVEAL Multicenter Randomized Clinical Trial. Surg Endosc (2023) 37:2143–53. 10.1007/s00464-022-09722-9
27.
Irfan A Cochrun S He K Okorji L Parmar AD . Towards Identifying a Learning Curve for Robotic Abdominal Wall Reconstruction: A Cumulative Sum Analysis. Hernia (2023) 27:671–6. 10.1007/s10029-023-02794-z
28.
Henriksen NA Marckmann M Christoffersen MW Jensen KK . Cost Analysis of Open Versus Robot-Assisted Ventral Hernia Repair. Author's Reply. Hernia (2024) 29:15. 10.1007/s10029-024-03206-6
Summary
Keywords
incisional hernia, umbilical hernia, readmission, length of stay, robotic surgery
Citation
Henriksen NA, Willaume Christoffersen M, Marckmann M and Jensen KK (2025) Procedural Costs of Robot-Assisted and Laparoscopic Ventral and Incisional Hernia Repair. A Propensity-Score Matched Nationwide Database Study. J. Abdom. Wall Surg. 4:15464. doi: 10.3389/jaws.2025.15464
Received
21 August 2025
Accepted
21 October 2025
Published
04 November 2025
Volume
4 - 2025
Updates
Copyright
© 2025 Henriksen, Willaume Christoffersen, Marckmann and Jensen.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nadia A. Henriksen, nadiahenriksen@gmail.com
ORCID: Nadia A. Henriksen, orcid.org/0000-0002-1805-9866
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.