Abstract
Background:
Hernia surgery requires precise technical skills to ensure successful patient outcomes. Traditional surgical training methods face challenges related to patient safety and limited operative exposure. Simulation training offers a risk-free platform to develop and refine surgical skills. This study evaluates the usefulness of simulation training for surgeons in hernia surgery.
Aim:
To assess the effectiveness of simulation training in enhancing the surgical skills and confidence of surgeons performing hernia repair.
Methods:
A prospective observational study was conducted with 44 surgical trainees undergoing simulation-based hernia surgery training. Technical skills and confidence levels were assessed before and after the training using standardized scoring systems. Participant feedback on the realism and applicability of simulation was also collected. Statistical analysis was performed using paired t-tests and chi-square tests.
Results:
Technical skill scores improved from a mean of 58.3(SD 8.4) pretraining, with a mean difference of 21.4, (95% Cl: 18.9 to 24.5, p < 0.001, effect size [Cohen’s d]∼2.1). Confidence scores increased from a mean of 4.2 (SD 1.5) to 7.8 (SD 1.2), with a mean difference of 3.6 (95% Cl: 3.1 to 4.3, p < 0.001, effect size [Cohen’s d}∼2.3). Over 85% of participants agreed that the simulation was realistic and beneficial for skill enhancement. Ninety-five percent recommended simulation training as a regular part of surgical education.
Conclusion:
In the study Simulation training significantly improves the technical proficiency and confidence of surgeons in hernia surgery. Its incorporation into surgical training programs is recommended to enhance operative readiness but further multicentric studies are needed to validate their results.
Introduction
Hernia surgery is one of the most commonly performed surgical procedures worldwide, encompassing various types such as inguinal, femoral, umbilical, and incisional hernias. The success of hernia repair depends on the surgeon’s skill, knowledge, and experience in both open and minimally invasive techniques. Traditionally, surgical skills were acquired through apprenticeship models involving direct observation and hands-on practice in the operating theatre under supervision [1]. However, this approach has limitations including patient safety concerns, limited operative exposure, and variability in learning curves. Consequently, modern surgical education emphasizes the importance of simulation training to improve technical skills before operating on patients [2, 3].
Simulation-based surgical training uses artificial models, virtual reality, and cadaveric or animal tissues to mimic clinical scenarios in a controlled, risk-free environment. It allows surgeons to practice and refine techniques repeatedly, receive feedback, and improve decision-making abilities without jeopardizing patient safety. For hernia surgery, simulation training provides an opportunity to master laparoscopic and open procedures, understand anatomical nuances, and learn to handle complications. Various simulation modalities such as box trainers, high-fidelity virtual reality simulators, and 3D-printed models are increasingly integrated into surgical curricula [4].
Kurashima, Khatib, Grantcharov have demonstrated that simulation training enhances the technical skills of surgeons, reduces the learning curve, improves operative performance, and positively influences patient outcomes [5–9]. Simulation also contributes to standardizing training, ensuring consistent skill acquisition irrespective of case volume or institutional resources. In addition, it fosters team communication and crisis management skills, which are crucial in complex surgical procedures [10].
Despite these advantages, the application of simulation training specifically in hernia surgery remains an evolving field. While laparoscopic hernia repair demands a high degree of technical proficiency, few studies have systematically evaluated the impact of simulation training on surgeons’ performance and clinical outcomes in hernia repairs. This research seeks to address this gap by assessing the usefulness of simulation-based training for surgeons performing hernia surgery at Apollo Simulation Centre, Chennai [11, 12].
Aim
This study was designed to evaluate the usefulness of simulation training in enhancing surgical skills and confidence among surgeons performing hernia repairs. Specifically, it assessed improvement in technical ability before and after structured training, measured changes in participants’ confidence levels, and analyzed participants feedback regarding the realism and applicability of simulation to surgical practice.
Materials and Methodology
Source of Data
The data for this study was obtained from participants undergoing simulation-based training sessions for hernia surgery conducted at the Apollo Simulation Centre, Vanagaram, Chennai.
Study Design
This was a prospective observational study involving multiple batches of surgical trainees undergoing structured simulation training in hernia surgery.
Study Location
The study was conducted at the Apollo Simulation Centre located in Vanagaram, Chennai, equipped with advanced surgical simulators and training modules.
Study Duration
The study was carried out over a period of 1 year from August 2022 to August 2023, involving four batches of participants.
Sample Size
A total of 44 participants were enrolled across four batches: Batch 1: 10 participants; Batch 2: 12 participants; Batch 3: 12 participants; Batch 4: 10 participants.
Inclusion Criteria
Surgeons and surgical trainees interested in enhancing their skills in hernia surgery.
Participants who consented to attend and complete the simulation training sessions.
Participants with basic knowledge of surgical anatomy and techniques related to hernia repair.
Participants who consented to use the data for research work.
Exclusion Criteria
Surgeons who had prior extensive experience (>50 hernia surgeries) in laparoscopic hernia repair.
Participants unwilling or unable to attend the full duration of training.
Those with contraindications for participation in simulation training (e.g., severe motion sickness with VR simulators).
Procedure and Methodology
Pre-Training Assessment: A structured, task- specific checklist and global rating scale (GRS) were used to evaluate technical performance. These tools were adapted from existing validated laparoscopic surgical assessment models such as the GOALS (Global Operative Assessment of Laparoscopic Skills) framework (Agha et al. [6]; Stefanidis et al. [13]). The checklist focussed on: port placement, instrument handling, tissue manipulation, mesh placement and fixation, endosuturing, hemostasis and complication management. Confidence was measured using a self-reported 10-points Likert scale, adapted from instruments used in previous surgical education studies (Shetty et al. [14]) and knowledge levels were assessed via questionnaires.
Simulation Training Sessions: Participants received hands-on training using high-fidelity laparoscopic simulators and synthetic anatomical models replicating inguinal and ventral hernias. Training included: Anatomical orientation and port placement. Mesh handling and fixation techniques. Management of intraoperative complications. Repetitive practice sessions with immediate feedback from expert faculty.
Post-Training Assessment: After completion of the training sessions, participants were reassessed with the same standardized metrics used during pre-training. Objective improvements in skills and knowledge were recorded.
Feedback Collection: Participants provided feedback on the simulation training’s usefulness, realism, and applicability to actual surgical practice through structured questionnaires and interviews.
Sample Processing
All assessment data and questionnaire responses were anonymized and compiled into a secured database. Skill performance scores were tabulated and statistically analyzed.
Statistical Methods
Descriptive statistics (mean, standard deviation) were used to summarize demographic data and performance scores.
Paired t-tests were employed to compare pre- and post-training skill scores and confidence levels. Chi-square tests assessed categorical variables from feedback questionnaires. Statistical significance was set at p < 0.05.
Data analysis was performed using SPSS version 25.0.
Data Collection
Data were collected through direct observation by faculty using validated scoring systems during simulated tasks, and through self-administered questionnaires on knowledge and confidence before and after training. All data were recorded in structured proformas and entered into electronic databases for analysis.
Observation and Results
Table 1 presents the baseline demographic and clinical characteristics of the 44 participants enrolled in the study. The mean age of participants was 32.7 years with a standard deviation of 6.8 years, indicating a relatively young cohort, and this was not statistically significant (t = 0.43, 95% CI: 31.1 to 34.3, p = 0.670). Male participants constituted the majority with 27 individuals (61.4%), while females accounted for 17 (38.6%), and this gender distribution showed no significant difference (χ2 = 0.41, 95% CI: 45.8%–70.2%, p = 0.523). Regarding prior experience with hernia surgery, 14 participants (31.8%) reported previous exposure, while the majority, 30 participants (68.2%), did not have such experience; however, this difference was not statistically significant (χ2 = 2.73, 95% CI: 19.7%–43.9%, p = 0.098). Notably, only 6 participants (13.6%) had prior simulation training exposure, whereas the vast majority (86.4%) had no such exposure, and this difference was statistically significant (χ2 = 10.1, 95% CI: 5.4%–21.8%, p = 0.001), highlighting that most participants were new to simulation training.
TABLE 1
| Parameter | Category/value | n (%) or mean (SD) | Test statistic (t/χ2) | 95% CI | P-value |
|---|---|---|---|---|---|
| Age (years) | — | 32.7 (6.8) | t = 0.43 | 31.1 to 34.3 | 0.670 |
| Gender | Male | 27 (61.4%) | χ2 = 0.41 | 45.8%–70.2% | 0.523 |
| Female | 17 (38.6%) | | | | |
| Previous hernia surgery experience | Yes | 14 (31.8%) | χ2 = 2.73 | 19.7%–43.9% | 0.098 |
| No | 30 (68.2%) | | | | |
| Simulation training | Yes | 6 (13.6%) | χ2 = 10.1 | 5.4%–21.8% | 0.001* |
| Exposure | No | 38 (86.4%) | | | |
Baseline demographic and clinical characteristics of participants (n = 44).
Symbol (*) denotes statistical significance (p < 0.05).
Table 2 compares the technical skills scores of participants before and after the simulation training. The pre-training mean score was 58.3 (SD 8.4), which significantly improved to a post-training mean of 79.6 (SD 7.1). The paired t-test showed a highly significant difference with t = 14.2, and the 95% confidence interval of the mean difference ranged from 18.9 to 24.5, with a p-value of less than 0.001. This indicates that simulation training markedly enhanced the technical skills of the participants.
TABLE 2
| Parameter | Pre-training mean (SD) | Post-training mean (SD) | Test statistic (t) | 95% CI of mean difference | P-value |
|---|---|---|---|---|---|
| Technical skills score (0–100) | 58.3 (8.4) | 79.6 (7.1) | t = 14.2 | 18.9 to 24.5 | <0.001* |
Technical skills score before and after simulation training (n = 44).
Symbol (*) denotes statistical significance (p < 0.05).
Table 3 assesses the participants’ confidence levels in performing hernia surgery before and after the training. The mean confidence score before training was 4.2 (SD 1.5) on a 0–10 scale, which increased significantly to 7.8 (SD 1.2) after training. The increase was statistically significant, with a t-value of 13.7, a 95% confidence interval for the difference between 3.1 and 4.3, and a p-value less than 0.001. These results demonstrate that simulation training significantly improved the surgeons’ self-reported confidence in performing hernia repairs.
TABLE 3
| Parameter | Pre-training mean (SD) | Post-training mean (SD) | Test statistic (t) | 95% CI of mean difference | P-value |
|---|---|---|---|---|---|
| Confidence score (0–10) | 4.2 (1.5) | 7.8 (1.2) | t = 13.7 | 3.1 to 4.3 | <0.001* |
Confidence levels before and after simulation training (n = 44).
Symbol (*) denotes statistical significance (p < 0.05).
Table 4 summarizes participant feedback regarding the effectiveness and applicability of the simulation training. A majority of participants (79.5%) agreed that the simulation was realistic, with 13.6% remaining neutral and 6.8% disagreeing (χ2 = 27.1, p < 0.001). Regarding the usefulness of the training for skill enhancement, 88.6% agreed, 6.8% were neutral, and 4.6% disagreed (χ2 = 34.5, p < 0.001). When asked about the applicability of the simulation to real surgical scenarios, 75% agreed, 18.2% were neutral, and 6.8% disagreed (χ2 = 21.8, p < 0.001). Importantly, 95.5% of participants recommended the continuation and expansion of simulation training in the future, with only 4.5% neutral and none disagreeing (χ2 = 40.0, p < 0.001). Overall, the feedback reflects a strong positive reception towards the simulation training’s realism, skill building utility, and relevance to actual surgery.
TABLE 4
| Feedback parameter | Agree n (%) | Neutral n (%) | Disagree n (%) | Test statistic (χ2) | P-value |
|---|---|---|---|---|---|
| Realism of simulation | 35 (79.5) | 6 (13.6) | 3 (6.8) | χ2 = 27.1 | <0.001* |
| Usefulness for skill enhancement | 39 (88.6) | 3 (6.8) | 2 (4.6%) | χ2 = 34.5 | <0.001* |
| Applicability to real surgery | 33 (75.0) | 8 (18.2) | 3 (6.8) | χ2 = 21.8 | <0.001* |
| Recommendation for future training | 42 (95.5) | 2 (4.5) | 0 (0) | χ2 = 40.0 | <0.001* |
Participant feedback on effectiveness and applicability of simulation training (n = 44).
Symbol (*) denotes statistical significance (p < 0.05).
Discussion
Baseline Demographics and Simulation Exposure
The mean age of participants was 32.7 years (SD 6.8), with a predominance of males (61.4%) (Table 1). This demographic distribution aligns with studies conducted by Zahiri HR et al. [1] and Kurashima Y et al. [5], where surgical trainees were generally in their early 30s, reflecting early career stages. A similar male predominance was reported by Kurashima Y et al. [5], consistent with the traditionally male dominated surgical workforce. The study also found that only 31.8% of participants had prior experience in hernia surgery, and a small proportion (13.6%) had prior simulation training exposure, indicating a largely novice group in simulation methodology. The low previous exposure to simulation mirrors findings from Nazari T et al. [15], emphasizing that simulation remains an emerging training tool in many centers. The statistically significant difference in prior simulation exposure (p = 0.001) suggests the necessity and relevance of introducing structured simulation programs.
Technical Skills Improvement
Significant improvement in technical skills was observed after simulation training, with mean scores increasing from 58.3 to 79.6 (p < 0.001) (Table 2). This improvement echoes findings from Kurashima et al. and Khatib et al. [7], which demonstrated improved operative performance following simulation training. While review article by Agha RA et al. [6] summarize that proficiency-based simulation training substantially reduced errors in laparoscopic skills. The magnitude of improvement supports the hypothesis that simulation offers a safe, reproducible method to accelerate the learning curve without risk to patients’ as demonstrated in systemic reviews and prospective trial [6, 8, 9].
Confidence Levels
Participants’ confidence scores increased significantly from 4.2 to 7.8 post-training (p < 0.001) (Table 3). Increased confidence following simulation is well-documented; Shetty S et al. [14] showed that simulation-trained residents reported greater readiness to perform procedures independently. This is critical because confidence directly correlates with operative performance and decision-making in the clinical setting, as highlighted by Stefanidis D et al. [13]. The enhancement in confidence also suggests improved cognitive assimilation of surgical techniques via simulation.
Participant Feedback
Feedback on the simulation’s realism, usefulness, applicability, and future recommendation was overwhelmingly positive, with 75%–95% agreement rates and significant chi-square results (all p < 0.001) (Table 4). This corroborates studies like Lorenz R et al. [16], which emphasized that trainees valued the fidelity and educational impact of simulation. The near-unanimous recommendation for future training underscores the growing consensus that simulation should be integral to surgical education, as supported by Sharma D et al. [17]. Participants found the simulation a realistic and effective tool for skill enhancement, which is essential for adoption and continued investment in simulation infrastructure.
Conclusion
In the study we found that the structured Simulation training proves to be a highly effective educational tool for enhancing the surgical skills and confidence of surgeons performing hernia surgery. The significant improvement in technical skills and self-reported confidence following simulation-based training underscores its value in surgical education (Figure 1). While these findings suggest potential for improving operative readiness our study didnot assess intraoperative performance or patient outcome. Incorporating structured simulation modules into surgical curricula can accelerate skill acquisition, reduce the learning curve. Therefore, simulation training should be considered an integral component of training programs for hernia surgery and future research should evaluate whether these improvements translate into clinical benefits.
FIGURE 1
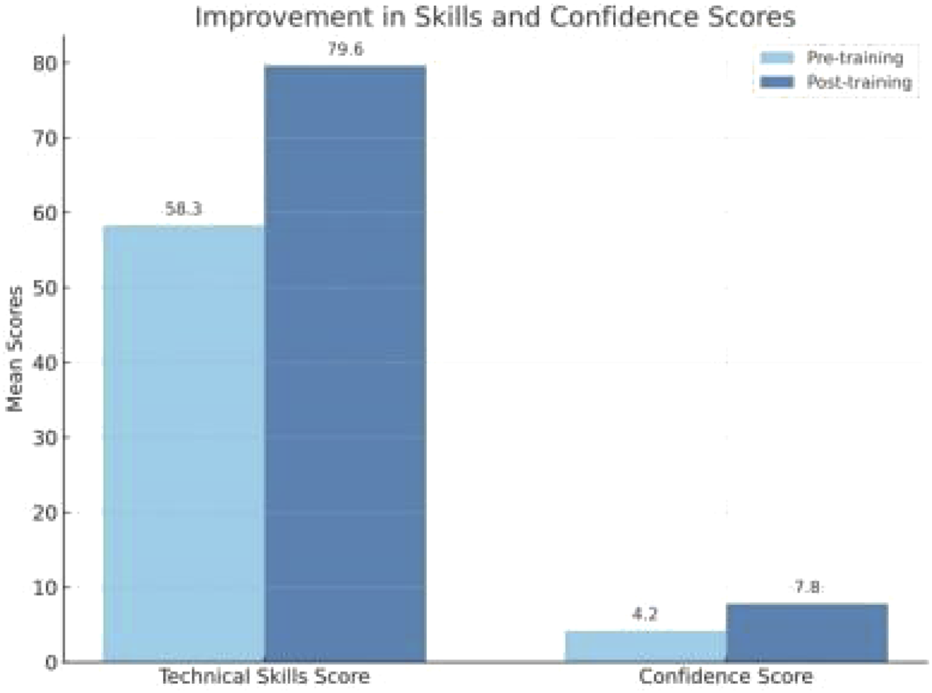
Improvement in skills and confidence scores.
Limitations of the Study
Despite promising results, this study has several limitations. The sample size of 44 participants, although adequate for preliminary assessment, limits the generalizability of the findings. The study was conducted at a single center with specific simulation equipment, which may not be representative of all training environments. Additionally, the assessment relied on simulated scenarios rather than real operative performance, so the direct translation of skills to clinical outcomes was not measured. The study’s relatively short follow-up period precludes evaluation of long-term skill retention. A control group was not included to differentiate between performance improvement due to the simulation training and the potential test retest learning effect. Lastly, participant self-assessment of confidence may be subject to bias. Future multicentric studies with larger cohorts and longitudinal follow-up are warranted to validate and expand upon these findings.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study involving human participants were reviewed and approved by Institutional Ethics Committee-Bio Medical Research, Apollo Hospitals, Chennai Tamilnadu. The participants provided written informed consent to participate in this study.
Author contributions
PB: Conceptualized the study, provided expert guidance, and contributed to the interpretation of the findings. PB also supervised the overall research process and reviewed the final manuscript. KW: Led the study design, methodology, and execution. KW also drafted and revised the manuscript, serving as the corresponding author. MM: Assisted in the study design and was involved in the analysis and interpretation of the data. MM contributed to the drafting of the manuscript and provided critical revisions. RP: Contributed to the study design and facilitated the statistical analysis. RP was also involved in the creation and assessment of simulation training modules and provided valuable feedback during manuscript development. VG and AM: Participated in the execution of the simulation training and contributed to data collection. They helped with data analysis and interpretation and provided critical revisions of the manuscript. TM: Coordinated the simulation training sessions, providing valuable insights on their effectiveness. AS and ED: Participated in the collection of participant feedback and helped analyse the data. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declared that financial support was not received for this work and/or its publication.
Conflict of interest
The author(s) declared that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declared that generative AI was not used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
ZahiriHRParkAEPughCMVassiliouMVoellerG. “See One, Do One, Teach One”: Inadequacies of Current Methods to Train Surgeons in Hernia Repair. Surg Endoscopy (2015) 29:2867–72. 10.1007/s00464-015-4411-7
2.
KöckerlingF. What Is the Influence of Simulation-Based Training Courses, the Learning Curve, Supervision, and Surgeon Volume on the Outcome in Hernia Repair? A Systematic Review. Front Surg (2018) 5:57. 10.3389/fsurg.2018.00057
3.
PellyTVance-DanielJLinderC. Characteristics of Laparoscopic and Open Hernia Repair Simulation Models: A Systematic Review. Hernia (2022) 26(1):39–46. 10.1007/s10029-021-02442-4
4.
Hernández-IrizarryRZendejasBAliSMFarleyDR. Optimizing Training Cost Effectiveness of Simulation-Based Laparoscopic Inguinal Hernia Repairs. The Am J Surg (2016) 211(2):326–35. 10.1016/j.amjsurg.2015.07.027
5.
KurashimaYFeldmanLSKanevaPAFriedGMBergmanSDemyttenaereSVet alSimulation-Based Training Improves the Operative Performance of Totally Extraperitoneal (TEP) Laparoscopic Inguinal Hernia Repair: A Prospective Randomized Controlled Trial. Surg Endoscopy (2014) 28:783–8. 10.1007/s00464-013-3241-8
6.
AghaRAFowlerAJ. The Role and Validity of Surgical Simulation. Int Surgery (2015) 100(2):350–7. 10.9738/INTSURG-D-14-00004.1
7.
KhatibMHaldNBrentonHBarakatMFSarkerSKStandfieldNet alValidation of Open Inguinal Hernia Repair Simulation Model: A Randomized Controlled Educational Trial. The Am J Surg (2014) 208(2):295–301. 10.1016/j.amjsurg.2013.12.007
8.
SpiliotisAESpiliotisPMPaliosIM. Transferability of Simulation‐Based Training in Laparoscopic Surgeries: A Systematic Review. Minimally Invasive Surgery (2020) 2020(1):5879485. 10.1155/2020/5879485
9.
GrantcharovTPReznickRK. Training Tomorrow’s Surgeons: The Role of Simulation in Surgical Education. Ann Surg (2008) 247(6):854–9. 10.1007/s10029-019-02093-6
10.
NazariTDankbaarMESandersDLAndereggMCWiggersTSimonsMP. Learning Inguinal Hernia Repair? A Survey of Current Practice and of Preferred Methods of Surgical Residents. Hernia (2020) 24:995–1002. 10.1007/s10029-020-02270-y
11.
SadavaEENovitskyYW. Simulation in Hernia Surgery: Where Do We Stand?J Laparoendoscopic and Adv Surg Tech (2021) 31(5):551–5. 10.1089/lap.2021.0081
12.
KöckerlingFSheenAJBerrevoetFCampanelliGCuccurulloDFortelnyRet alThe Reality of General Surgery Training and Increased Complexity of Abdominal Wall Hernia Surgery. Hernia (2019) 23:1081–91. 10.1007/s10029-019-02062-z
13.
StefanidisDSevdalisNPaigeJZevinBAggarwalRGrantcharovTet alSimulation in Surgery: What’s Needed Next?Ann Surgery (2015) 261(5):846–53. 10.1097/SLA.0000000000000826
14.
ShettySZevinBGrantcharovTPRobertsKEDuffyAJ. Perceptions, Training Experiences, and Preferences of Surgical Residents Toward Laparoscopic Simulation Training: A Resident Survey. J Surg Education (2014) 71(5):727–33. 10.1016/j.jsurg.2014.01.006
15.
NazariTSimonsMPZebMHvan MerriënboerJJLangeJFWiggersTet alValidity of a Low-Cost Lichtenstein Open Inguinal Hernia Repair Simulation Model for Surgical Training. Hernia (2020) 24:895–901. 10.1007/s10029-019-02093-6
16.
LorenzRStechemesserBReinpoldWFortelnyRMayerFSchröderWet alDevelopment of a Standardized Curriculum Concept for Continuing Training in Hernia Surgery: German Hernia School. Hernia (2017) 21:153–62. 10.1007/s10029-016-1566-7
17.
SharmaDAgrawalVBajajbJAgarwalaP. Low-Cost Simulation Systems for Surgical Training: A Narrative. J Surg Simulation (2020) 5:1–20. 10.1089/lap.2016.0644
Summary
Keywords
hernia surgery, laparoscopic, simulation training, surgical skills enhancement, Apollo hospital
Citation
Balachandran P, Waykole KP, Manikesi M, Palaniappan R, Gubendran V, Manimaran A, Muthiah T, Somasundaram A and DurgaDevi E (2026) Role of Simulation Training in Hernia Surgery and Abdominal Wall Reconstruction. J. Abdom. Wall Surg. 4:15274. doi: 10.3389/jaws.2025.15274
Received
15 July 2025
Revised
08 September 2025
Accepted
15 December 2025
Published
08 January 2026
Volume
4 - 2025
Updates
Copyright
© 2026 Balachandran, Waykole, Manikesi, Palaniappan, Gubendran, Manimaran, Muthiah, Somasundaram and DurgaDevi.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kanchan Pankaj Waykole, kanchaningle2009@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.