Introduction
In the last few decades, surgery has become a fast-evolving field, where new technologies are introduced rapidly and spread across the various surgical sub-specialities. Among them, robotic surgery is one such technology, and its use is increasing, especially in the field of hernia surgery. Its fast adoption was to provide an alternative to open surgery by enhancing surgeons’ dexterity and ergonomics by utilising seven degrees of freedom and 3D vision, and also providing a significant advantage in restricted space like the pelvis and retromuscular plane, in which accurate dissection and suturing was a big challenge even for the more skilful surgeons. Ultimately, this resulted in an overall increase in the usage of minimally invasive hernia surgeries and related benefits for the patients [1]. While many surgeons today have embraced robotic surgery, there remains scepticism regarding cost-efficiency and long-term benefits [2].
Technical and Ergonomic Advantages of Surgical Robotic Devices
Surgical robotic technology has advanced from mere passive robots used for retraction or holding instruments like rail-mounted devices or camera navigation to active robotic systems such as the Da Vinci Surgical system, Hugo Medtronic, Medicaid Hinotori, Versius CMR, and many more, which range of motion of surgical instruments enables high performance and enhanced precision for dissection, suturing the abdominal wall using a minimally invasive approach [3]. Furthermore, it eliminates physiological tremors and the fulcrum effect present in laparoscopic surgery. The wristed instruments of the robot provide several degrees of freedom to overcome the limitation of traditional laparoscopic instruments which often do not permit the tip of the instrument to reach the anterior abdominal wall [4] and allow suturing in challenging ergonomic positions. Thus, by utilising the robot, intracorporeal primary closure of fascial defect [5] and intraperitoneal placement of mesh are performed with greater ease and high success rate [6].
Surgeons who perform minimally invasive surgery are more likely to experience neck and shoulder pain compared to surgeons performing open surgery [7] because they tend to hold their neck in a static posture while simultaneously isometrically contracting the shoulder muscles in an abducted position during long operations [8]. On the contrary, in robotic surgery, the surgeon is seated at the console visualising the surgical field through a viewfinder while manipulating the hand controls and foot pedals to control the surgical instruments. Thus, with improved ergonomics, this reduces the risk of fatigue and backache [9]. Nevertheless, it is important to utilise proper posture and equipment setup as improper posture while performing robotic surgery can still lead to muscle aches and eye strain [10]. However, the option to set up your setting will minimise those health hazards.
Reduced Complications
Inguinal Hernia Surgery
Multiple systematic reviews comparing robotic hernia surgery to laparoscopic or open surgery have shown reduced risks of complications in patients who underwent robotic surgery. De Angelis et al.‘s systematic review with pooled data analysis from 58 meta-analyses has shown that robotic inguinal hernia surgery was associated with a lower rate of hernia recurrences and conversion to open surgery compared to laparoscopic surgery [11]. Waitre et al. have reported reduced postoperative pain scores in robotic-assisted transabdominal preperitoneal repair compared to the conventional laparoscopic approach [12]. Yet, the RIVAL trial showed that for straightforward inguinal hernia, there was no clinical benefit using the robotic approach compared to the laparoscopic approach, and the robotic approach cost more, had longer operative time, and was associated with higher surgeon frustration with no ergonomic benefit to the surgeon [13].
With regards to robotic vs. open inguinal hernia, De Angelis et al.‘s systematic review has shown that robotic inguinal hernia repair was associated with fewer surgical site infections, less intraoperative blood loss, and shorter postoperative length of stay compared to open inguinal hernia repairs [11]. Bittner et al. showed significantly lower postoperative pain scores for laparoscopic and robotic inguinal hernia repair compared to open repairs [14]. Table 1 summarises the conclusions from the above studies discussed. Still, better-designed trials looking not only at patients’ perspectives but also at surgeons’ benefits are needed to fully resolve the issues. Significantly, robotic inguinal hernia repair has brought more surgeons to adopt the use of endolaparoscopic/robotic repair for inguinal hernia, a technique that was slowly adopted in the past.
TABLE 1
| Paper | Type of study | Conclusion |
|---|---|---|
| De Angelis et al. 2023 [11] | Systematic review | The robotic inguinal hernia was associated with lower rates of hernia recurrences and conversion to open surgery compared to the laparoscopic approach |
| However, the robotic approach required a longer operative time | ||
| Waite et al. 2016 [12] | Retrospective study | Robotic TAPP repair had lower postoperative pain than laparoscopic TAPP repair |
| However, robotic TAPPP required longer operative time and costs more | ||
| Prabhu et al. 2020 RIVAL trial [13] | Randomised Clinical Trial | Robotic inguinal hernia repair was associated with increased operative time, cost, and surgeon frustration without discernible ergonomic benefit for the surgeons, compared to laparoscopic repair |
| Bittner et al. 2018 [14] | Prospective study | Robotic inguinal hernia repair was associated with lower postoperative pain at 1 week, lesser activity disruption at 1 week, and shorter duration of analgesia use compared to open repair |
| Robotic inguinal hernia repair had similar postoperative pain and activity restrictions at 1 week compared to laparoscopic repair |
Studies analysing outcomes from robotic inguinal hernia repair compared with open and laparoscopic approaches.
TAPP, transabdominal preperitoneal.
Ventral Hernia Surgery
In our institution, robotic extended totally extraperitoneal repair (eTEP) paraumbilical hernia and rectus diastasis repair is commonly performed. Figure 1 depicts a cross-over to dissect both retro-rectus spaces. Figure 2 depicts intraoperative suturing for the apposition of the rectus muscles. Figure 3 depicts mesh placement in the retrorectus space. The ease of intracorporeal suturing using a robot vs. laparoscopic approach facilitates surgery for larger hernias.
FIGURE 1
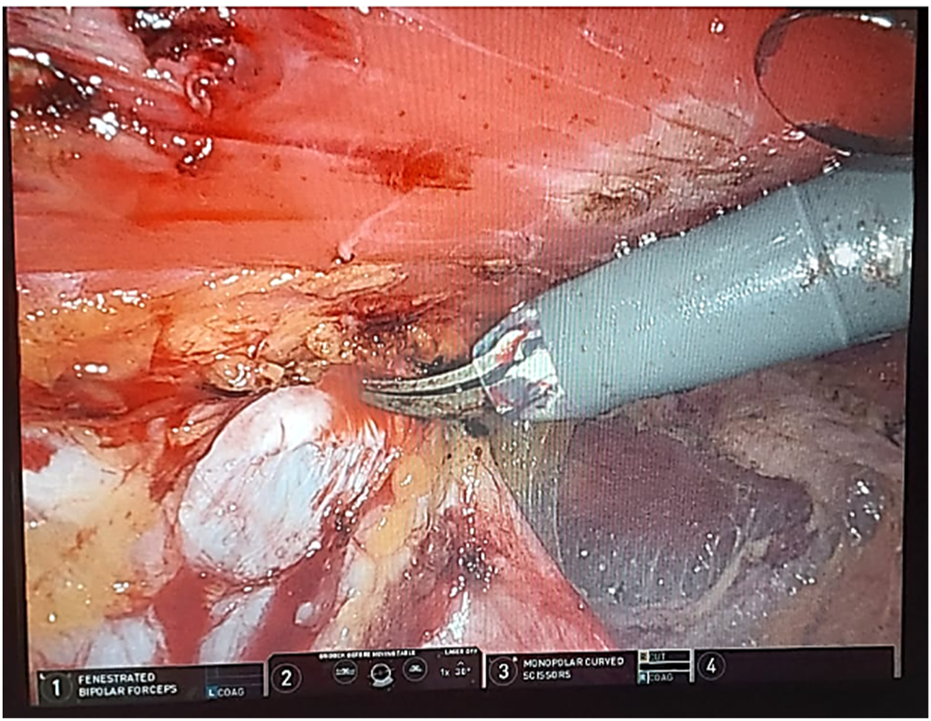
Depicts a cross-over to dissect both retro-rectus spaces.
FIGURE 2
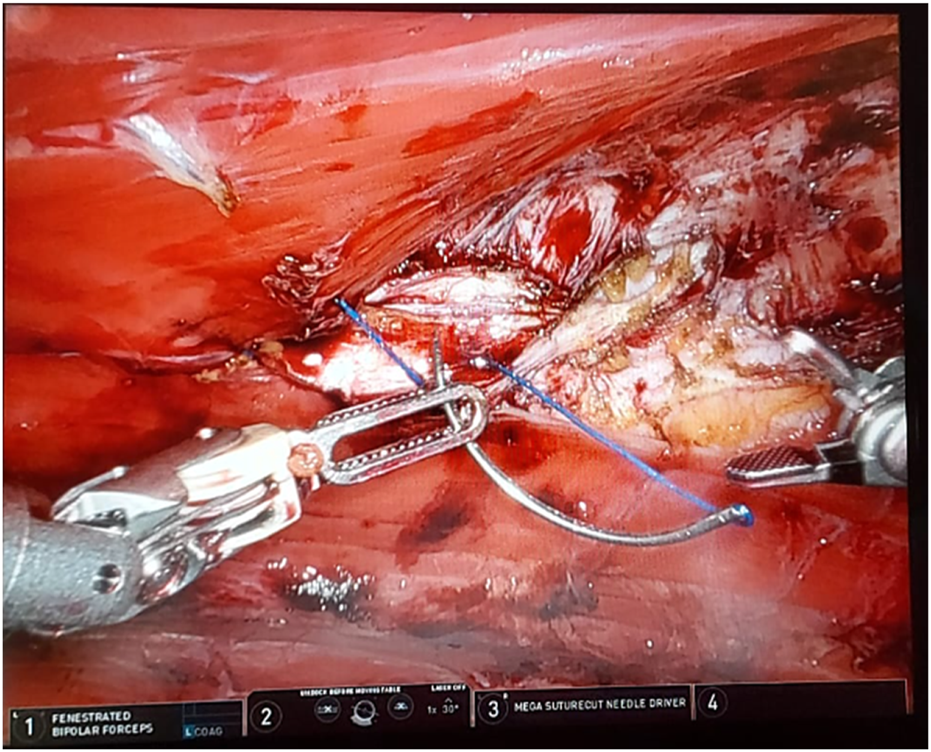
Depicts intraoperative suturing for the apposition of the rectus muscles.
FIGURE 3
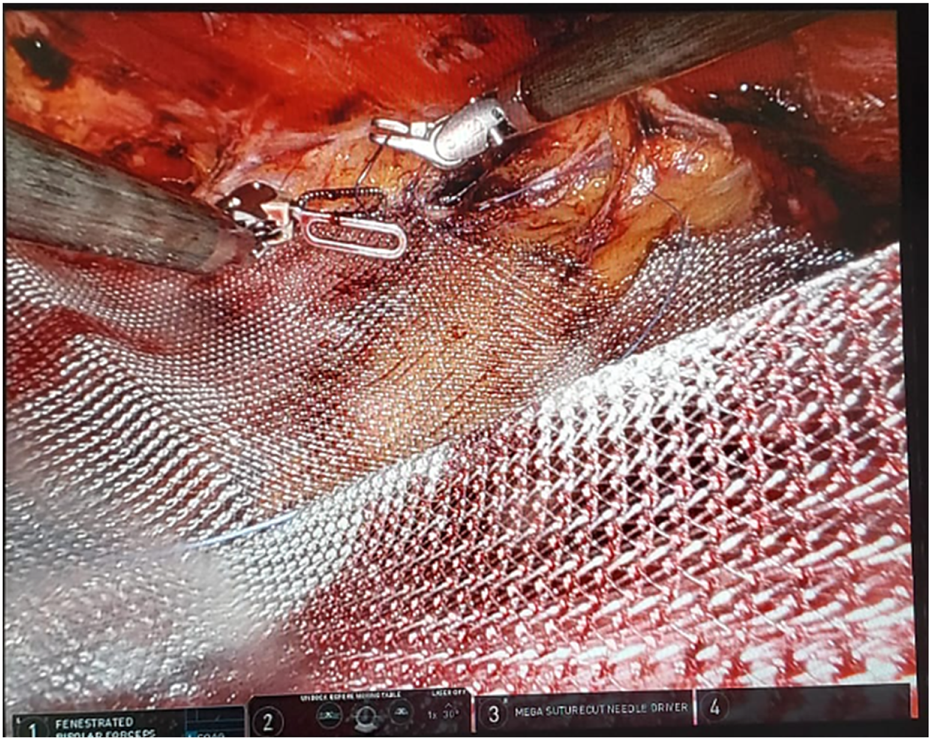
Depicts mesh placement in the retrorectus space.
Yet, there have been varied results of robot-assisted hernia repair compared to laparoscopic and open repair. The challenges in ventral hernia repair, the rise of new technical approaches for ventral hernia repair, and the benefits of the robotic technology itself are all factors that have significantly contributed to the wide adoption and success of robotic ventral hernia repair, especially in the United State. The American database from Inpatient Sample found no difference in postoperative complications between robotic vs. laparoscopic ventral hernia repair [15], but the American Hernia Society Quality Collaborative showed fewer postoperative complications in robot-assisted intraperitoneal mesh placement (IPOM) vs. laparoscopic IPOM [16]. One of the main advantages resulting from utilising the robotic device in ventral hernia repair is that it can facilitate the placement of the mesh in the extraperitoneal space, avoiding possible related complications of an intraperitoneal mesh coming in contact with the bowel. Moreover, it has the possibility of approximating the recti muscles by closing the hernia defect and reconstituting the lines alba for better functionality of the abdominal wall. However, a systematic review showed that extra-peritoneal mesh does not appear to be superior to intraperitoneal mesh in the short term for minimally invasive ventral hernia repair [17]. Fascial closure was achieved in more than 90% of robotic ventral hernia cases compared to 50% of laparoscopic ventral hernia repairs. This was achieved largely with enhanced suturing in the robotic cases compared with tacks and sutures in the laparoscopic group [18]. Sutured closure of hernia defect reduces recurrence rates of bulging, pseudo-recurrence, and seroma formation [19]. Therefore, the robot proved to be useful in increasing the rate of achieved defect closure [20]. There were significantly smaller bowel injuries in the laparoscopic group compared with robotic ventral hernia repair [11, 21]. The length of postoperative stay was shorter for robotic ventral hernia compared to laparoscopic ventral hernia repair [22]. Yet, the PROVE-IT randomised clinical trial has shown comparable outcomes between laparoscopic and robotic ventral hernia mesh repair, and the increased operative time and cost of robotic ventral hernia surgery were not offset by a measurable clinical benefit [23]. Table 2 summarises the conclusions from the above studies.
TABLE 2
| Paper | Type of study | Conclusion |
|---|---|---|
| De Angelis et al. 2023 [11] | Systematic review | Robotic ventral hernia was associated with lower rates of bowel injuries and conversion to open surgery compared to the laparoscopic approach |
| The robotic ventral hernia was associated with lower postoperative complications, lower surgical site infections, lesser intraoperative blood loss, and shorter postoperative stay than open surgery | ||
| However, the robotic approach required a longer operative time | ||
| Coakley et al. 2017 [15] | Retrospective study | Robotic ventral hernia repair was performed in older patients with more chronic conditions and cost more compared to the laparoscopic approach |
| Prabhu et al. 2017 [16] | Prospective study | Robotic IPOM was associated with a lower risk of surgical site infections and lower median length of stay than laparoscopic IPOM. |
| However, operative time was longer in robotic IPOM than laparoscopic approach | ||
| Walker et al. 2018 [20] | Retrospective study | Robotic ventral hernia repair was associated with a decreased incidence of recurrence and surgical site infection compared to the laparoscopic approach |
| The robotic approach was associated with increased primary fascial closure than the laparoscopic approach | ||
| Alfredo et al. 2018 [21] | Prospective study | Robotic ventral hernia repair was associated with a shorter length of stay than the open approach, but no significant differences were found for surgical site infections and 30-day readmission |
| Henriksen et al. 2019 [22] | Metanalysis | Robotic ventral hernia repair was associated with a shorter length of stay, but longer operative duration than the open approach |
| No significant differences in postoperative complications | ||
| Petro et al. 2021 PROVE-IT [23] | Randomised Clinical Trial | No significant differences in postoperative pain, quality of life, and length of hospital stay between robotic and laparoscopic ventral hernia repair |
Studies analysing outcomes from robotic ventral hernia repair compared with open and laparoscopic approaches.
IPOM, intraperitoneal mesh placement.
Surgical Robot in Transversus Abdominis Release (Robo-TAR)
As stated, Surgical Robotics not only allows retromuscular ventral hernia repair but also enables abdominal wall reconstruction and extraperitoneal mesh placement that was previously only possible with open repair by reducing wound morbidity [24], with shorter postoperative stay [25]. Overall, robotic devices also allow for additional procedures like posterior component separation and transverses abdomen release to allow the closure of large abdominal defects that was possible only with the open approach. Despite the increased mean operative time for robotic TAR compared to open TAR repair, mean blood loss was lower in patients who underwent robotic TAR [19]. A systematic review showed that there were no statistical differences between robotic vs. open TAR repair in terms of re-operation rates, surgical site infections, and readmissions [26]. Table 3 summarises the above studies on robotic TAR versus the open approach.
TABLE 3
| Paper | Type of study | Conclusion |
|---|---|---|
| Warren et al. 2017 [24] | Prospective study | Robotic ventral hernia was associated with increased rates of fascial closure and extraperitoneal mesh placement compared with the laparoscopic approach in which mesh was placed intraperitoneally |
| Longer operative duration for the robotic approach compared with the laparoscopic approach | ||
| The robotic approach was associated with increased seroma than the laparoscopic approach, but surgical site infection rates and narcotic requirements were similar | ||
| The length of postoperative hospital stay was shorter with the robotic approach | ||
| Direct hospital costs were similar between the robotic and laparoscopic approaches | ||
| Dewulf et al. 2022 [25] | Prospective study | Robotic TAR was associated with shorter postoperative stays and lower surgical site infections than open TAR. |
| However, there were similar reoperation and recurrence rates between robotic and open approaches | ||
| Martin-del-Campo et al. 2017 [19] | Prospective study | Open TAR was performed for patients with more comorbidities compared to robotic TAR. Average operative duration was longer in robotic TAR, but average blood loss was lower, compared to open TAR. No differences in surgical site infections between the two approaches |
| The length of postoperative stay was shorter for robotic TAR compared to the open approach | ||
| Bracale et al. 2021 [26] | Metanalysis | Robotic TAR was associated with a lower risk of complications and shorter postoperative stay, but longer operative duration compared to open TAR. |
| There were no differences in rates of surgical site infections, readmission, and reoperation rates |
Studies analysing outcomes from robotic TAR compared with the open approach.
TAR, transversus abdominus release.
Disadvantages of Surgical Robotic Devices
Operative time was significantly longer for robotic hernia surgery compared with the open and laparoscopic approach [11, 27]. The time needed to dock the robot could have contributed to the longer procedure time in robotic surgery. There is currently inadequate evidence to show that the higher usage of the robot in experienced centres results in a lower docking time that may translate to comparable operative duration with laparoscopic surgery [11].
A significant factor to consider is the high cost of investing in the robotic device coupled with the cost of annual maintenance and per-case utilisation [27]. Further studies are needed to justify the cost-effectiveness of robot use in hernia surgery. These studies may consider focusing on quantifying cost savings from the reduced length of stay, and lower rate of postoperative complications juxtaposed to the increased cost of dedicated operating theatre, trained nursing staff, and cost of equipping healthcare professionals to utilise the robot effectively [28].
Specialised training can be time-consuming and may not be readily available in certain medical institutions. Apart from training surgeons to use the robotic consoles, training of adept assistants is required to reduce robot docking time and effectively facilitate surgery [29].
However, a few single-centre series have shown that robot-assisted transabdominal preperitoneal, total extraperitoneal (TEP), and single-site TEP repairs were feasible without a high-learning curve for a laparoscopic surgeon [12].
Lastly, the availability of robotic surgery may be limited in certain geographic locations. Thus, fewer patients are offered robotic surgery, which in turn results in the surgeon performing fewer robotic hernia repairs compared to laparoscopic vs. open hernia repair. However, robotic surgery coupled with 5G internet allows telesurgery to be performed, allowing the operating surgeon to operate remotely from the patient [30].
Discussion
The use of robotic surgery enhances the possibility of repair in ventral hernia surgery which is expanding worldwide, especially with the adoption of newer techniques in hernia repair. It facilitates the shift from open surgery to a minimally invasive technique that has led to an increased percentage of adoption of endo-laparoscopic hernia repair. It has proven to have better clinical outcomes, especially in ventral hernias and complicated inguinal hernias. It facilitates the adoption of minimally invasive procedures but also facilitates surgery via extraperitoneal and retromuscular approaches that are technically demanding and difficult with the traditional endo-laparoscopic approach. Nevertheless, there is a need to evaluate the long-term outcome and cost-effectiveness of robotic hernia repair and determine if robotic hernia repair should be offered to all patients as a standard procedure. It is still a fascinating technology that requires a deep-quality study analysis by experts and academics.
Statements
Author contributions
DL and LT drafted the manuscript. SW supplied the photos. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Sheetz KH Claflin J Dimick JB . Trends in the Adoption of Robotic Surgery for Common Surgical Procedures. JAMA Netw open (2020) 3(1):e1918911. 10.1001/jamanetworkopen.2019.18911
2.
Telem DA . Is Robotic Surgery the Future for Abdominal Wall Hernia Repair? Not So Fast. Ann Surg (2018) 267(2):218–9. 10.1097/SLA.0000000000002336
3.
Bittner JG Alrefai S Vy M Mabe M Del Prado PAR Clingempeel NL . Comparative Analysis of Open and Robotic Transversus Abdominis Release for Ventral Hernia Repair. Surg Endosc (2017) 32:727–34. 10.1007/s00464-017-5729-0
4.
Ballantyne GH Hourmont K Wasielewski A . Telerobotic Laparoscopic Repair of Incisional Ventral Hernias Using Intraperitoneal Prosthetic Mesh. JSLS: J Soc Laparoendoscopic Surgeons (2003) 7(1):7–14.
5.
Allison N Tieu K Snyder B Pigazzi A Wilson E . Technical Feasibility of Robot-Assisted Ventral Hernia Repair. World J Surg (2012) 36(2):447–52. 10.1007/s00268-011-1389-8
6.
Sugiyama G Chivukula S Chung PJ Alfonso A . Robot-Assisted Transabdominal Preperitoneal Ventral Hernia Repair. JSLS: J Soc Laparoendoscopic Surgeons (2015) 19(4):e2015.00092. 10.4293/JSLS.2015.00092
7.
Stucky CH Cromwell KD Voss RK Chiang YJ Woodman K Lee JE et al Surgeon Symptoms, Strain, and Selections: Systematic Review and Meta-Analysis of Surgical Ergonomics. Ann Med Surg (2018) 27:1–8. 10.1016/j.amsu.2017.12.013
8.
Park A Lee G Seagull FJ Meenaghan N Dexter D . Patients Benefit While Surgeons Suffer: An Impending Epidemic. J Am Coll Surgeons (2010) 210(3):306–13. 10.1016/j.jamcollsurg.2009.10.017
9.
Sanchez A Rodriguez O Jara G Sanchez R Vegas L Rosciano J et al Robot-Assisted Surgery and Incisional Hernia: A Comparative Study of Ergonomics in a Training Model. J Robot Surg (2018) 12:523–7. 10.1007/s11701-017-0777-y
10.
Tetteh E Wang T Kim J Smith T Norasi H Van Straaten MG et al Optimizing Ergonomics During Open, Laparoscopic, and Robotic-Assisted Surgery: A Review of Surgical Ergonomics Literature and Development of Educational Illustrations. AJS: Am J Surg (2023). 10.1016/j.amjsurg.2023.11.005
11.
de’Angelis N Schena CA Moszkowicz D Kuperas C Fara R Gaujoux S et al Robotic Surgery for Inguinal and Ventral Hernia Repair: A Systematic Review and Meta-Analysis. Surg Endosc (2023) 38:24–46. 10.1007/s00464-023-10545-5
12.
Waite KE Herman MA Doyle PJ . Comparison of Robotic Versus Laparoscopic Transabdominal Preperitoneal (TAPP) Inguinal Hernia Repair. J Robot Surg (2016) 10(3):239–44. 10.1007/s11701-016-0580-1
13.
Prabhu AS Carbonell A Hope W Warren J Higgins R Jacob B et al Robotic Inguinal vs Transabdominal Laparoscopic Inguinal Hernia Repair: The RIVAL Randomized Clinical Trial. JAMA Surg (2020) 155(5):380–7. 10.1001/jamasurg.2020.0034
14.
Bittner Iv JG Cesnik LW Kirwan T Wolf L Guo D . Patient Perceptions of Acute Pain and Activity Disruption Following Inguinal Hernia Repair: A Propensity-Matched Comparison of Robotic-Assisted, Laparoscopic, and Open Approaches. J Robot Surg (2018) 12:625–32. 10.1007/s11701-018-0790-9
15.
Coakley KM Sims SM Prasad T Lincourt AE Augenstein VA Sing RF et al A Nationwide Evaluation of Robotic Ventral Hernia Surgery. Am J Surg (2017) 214(6):1158–63. 10.1016/j.amjsurg.2017.08.022
16.
Prabhu AS Dickens EO Copper CM Mann JW Yunis JP Phillips S et al Laparoscopic vs Robotic Intraperitoneal Mesh Repair for Incisional Hernia: An Americas Hernia Society Quality Collaborative Analysis. J Am Coll Surg (2017) 225:285–93. 10.1016/j.jamcollsurg.2017.04.011
17.
Yeow M Wijerathne S Lomanto D . Intraperitoneal Versus Extraperitoneal Mesh in Minimally Invasive Ventral Hernia Repair: A Systematic Review and Meta-Analysis. Hernia (2022) 26:533–41. 10.1007/s10029-021-02530-5
18.
Gonzalez AM Romero RJ Seetharamaiah R Gallas M Lamoureux J Rabaza JR . Laparoscopic Ventral Hernia Repair With Primary Closure Versus No Primary Closure of the Defect: Potential Benefits of the Robotic Technology. Int J Med Robot (2015) 11(2):120–5. 10.1002/rcs.1605
19.
Martin-Del-Campo LA Weltz AS Belyansky I Novitsky YW . Comparative Analysis of Perioperative Outcomes of Robotic Versus Open Transversus Abdominis Release. Surg Endosc (2018) 32(2):840–5. 10.1007/s00464-017-5752-1
20.
Walker PA May AC Mo J Cherla DV Santillan MR Kim S et al Multicenter Review of Robotic Versus Laparoscopic Ventral Hernia Repair: Is There a Role for Robotics? Surg Endosc (2018) 32(4):1901–5. 10.1007/s00464-017-5882-5
21.
Carbonell AM Warren JA Prabhu AS Ballecer CD Janczyk RJ Herrera J et al Reducing Length of Stay Using a Robotic-Assisted Approach for Retromuscular Ventral Hernia Repair: A Comparative Analysis From the Americas Hernia Society Quality Collaborative. Ann Surg (2017) 267:210–7. 10.1097/SLA.0000000000002244
22.
Henriksen NA Jensen KK Muysoms F . Robot-Assisted Abdominal Wall Surgery: A Systematic Review of the Literature and Meta-Analysis. Hernia: J hernias Abdom wall Surg (2019) 23(1):17–27. 10.1007/s10029-018-1872-3
23.
Petro CC Zolin S Krpata D Alkhatib H Tu C Rosen MJ et al Patient-Reported Outcomes of Robotic vs Laparoscopic Ventral Hernia Repair With Intraperitoneal Mesh: The PROVE-IT Randomized Clinical Trial. JAMA Surg (2021) 156(1):22–9. 10.1001/jamasurg.2020.4569
24.
Warren JA Cobb WS Ewing JA Carbonell AM . Standard Laparoscopic Versus Robotic Retromuscular Ventral Hernia Repair. Surg Endosc (2017) 31(1):324–32. 10.1007/s00464-016-4975-x
25.
Dewulf M Hiekkaranta JM Mäkäräinen E Saarnio J Vierstraete M Ohtonen P et al Open Versus Robotic-Assisted Laparoscopic Posterior Component Separation in Complex Abdominal Wall Repair. BJS open (2022) 6(3):zrac057. 10.1093/bjsopen/zrac057
26.
Bracale U Corcione F Neola D Castiglioni S Cavallaro G Stabilini C et al Transversus Abdominis Release (TAR) for Ventral Hernia Repair: Open or Robotic? Short-Term Outcomes From a Systematic Review With Meta-Analysis. Hernia: J hernias Abdom wall Surg (2021) 25(6):1471–80. 10.1007/s10029-021-02487-5
27.
Scheuermann U Niebisch S Lyros O Jansen-Winkeln B Gockel I . Transabdominal Preperitoneal (TAPP) Versus Lichtenstein Operation for Primary Inguinal Hernia Repair—A Systematic Review and Meta-Analysis of Randomized Controlled Trials. BMC Surg (2017) 17(1):55. 10.1186/s12893-017-0253-7
28.
Ceresoli M Pisano M Abu-Zidan F Allievi N Gurusamy K Biffl WL et al Minimally Invasive Surgery in Emergency Surgery: A WSES Survey. World J Emerg Surg (2022) 17(1):18. 10.1186/s13017-022-00419-x
29.
Reinisch A Liese J Padberg W Ulrich F . Robotic Operations in Urgent General Surgery: A Systematic Review. J Robot Surg (2022) 17:275–90. 10.1007/s11701-022-01425-6
30.
Barba P Stramiello J Funk EK Richter F Yip MC Orosco RK . Remote Telesurgery in Humans: A Systematic Review. Surg Endosc (2022) 36(5):2771–7. 10.1007/s00464-022-09074-4
Summary
Keywords
robotic surgery, hernia, inguinal hernia, ventral hernia, robotic platform
Citation
Lomanto D, Tan L, Lee S and Wijerathne S (2024) Robotic Platform: What It Does and Does Not Offer in Hernia Surgery. J. Abdom. Wall Surg. 3:12701. doi: 10.3389/jaws.2024.12701
Received
17 January 2024
Accepted
29 January 2024
Published
14 February 2024
Volume
3 - 2024
Updates
Copyright
© 2024 Lomanto, Tan, Lee and Wijerathne.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Davide Lomanto, surdl@nus.edu.sg
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.