Abstract
In dynamic healthcare environments including the COVID-19 pandemic, it is paramount to communicate health recommendations expediently and clearly. Research has shown social determinants of health affect the impact of COVID-19 on abdominal transplant recipients, but there has been less research on the effect of language proficiency. This is a cohort study of time to first COVID-19 vaccination among abdominal organ transplant recipients in an academic medical center in Boston, MA between 18 December 2020, and 15 February 2021. Cox proportional hazards analysis of time to vaccination by preferred language were adjusted for race, age group, insurance, and transplanted organ. Among 3001 patients, 53% were vaccinated during the study period. Language preference other than English was independently associated with delay to vaccination (0.64, p = 0.001), on adjusted analysis. In addition, Black, Hispanic and other race patients were less likely to be vaccinated than white patients (0.58, 0.67, 0.68 vs. reference, all p < 0.03). Language preference other than English is an independent barrier to solid abdominal organ transplant recipients’ access to timely COVID-19 vaccination. Equity in care should be improved by providing targeted services to minority language speakers.
Introduction
Limited English proficiency (LEP) is increasingly recognized as an independent barrier to timely healthcare access and optimal outcomes (1–3). In the context of the dynamic COVID-19 pandemic, healthcare communication with the public is vital for timely access to testing, treatment, and vaccination. Prior research has established that patients with LEP, even within racial groups, have increased risk of contracting COVID-19, and of needing hospitalization after a positive COVID-19 test (4–6). A rubric has been proposed for improving clinical care of patients with LEP who test positive for COVID (7). However, it can be difficult to determine the contributory effect from various social determinants of health as patients with LEP may also have socioeconomic barriers to accessing timely healthcare.
Solid organ transplant recipients have been shown to have an elevated risk of testing positive for COVID-19, and of morbidity and mortality from the effects of the virus (8,9). Fortunately, these patients often receive long-term follow-up care from their transplant institution and thus are connected to a healthcare institution and hence more likely than the general population to receive targeted healthcare communication. Vaccinations against COVID-19 received U.S. Food and Drug Administration Emergency Use Authorization on 11 December 2020, but doses were limited. Abdominal solid organ recipients were identified early as a priority group to vaccinate. Abdominal organ transplant recipients receiving care at an academic medical center in Boston, MA were notified of their eligibility by email notice from their transplant team at the medical center in English and Spanish on 22nd January 2021, and paper notices were mailed, starting the same day. These vaccine doses were available for administration only via the academic medical center, as this was prior to vaccine availability in community-based vaccination centers. This study analyzes factors that affected time to vaccination for solid organ transplant patients upon vaccine eligibility, to assess for a disparity in access to timely vaccination among this immunosuppressed population who has established care with the transplant care team.
Materials and Methods
Data Source, Inclusion, and Exclusion Criteria
Abdominal organ (kidney or liver) transplant recipients receiving care at an academic medical center in Boston, MA were examined through the institutional electronic medical record (EMR) in this study. Patients were included who had a liver transplant, kidney transplant, or both organs. Patients were excluded if they did not have contact with the transplant care team in the past year or have missing data.
Primary Variables
Patients’ preferred language was the primary independent variable and was divided into two groups, English or language other than English. Date of first dose was used as the primary end point. Start day was the date the first participant in the study population received their first vaccination dose, 18th December 2020. In Massachusetts, COVID vaccinations began 15th December 2020 with healthcare workers, then were extended in stages to care facility residents, elderly and those with certain medical conditions including solid organ transplant recipients. Institutional medical interpreters were overloaded with clinical interpreting for the high census of inpatient COVID patients at the time, but the transplant clinic wanted to share this availability with patients as soon as possible. Bilingual clinic staff translated the notice into Spanish as this was the most commonly spoken non-English language among this population. Patients were notified of the availability of COVID-19 vaccine doses and their eligibility via dual language email and paper notices sent in both English and Spanish on 22nd January 2021. These vaccine doses were available for administration only via the academic medical center, as this was prior to vaccine availability in community-based vaccination centers. Patients were censored on 15th February 2021, which coincided with an institutional pause in vaccination due to decrease in supply.
Statistical Analysis
Factors associated with prolonged time to first vaccination in days were adjusted by the cox proportional hazard model, including sex, race, age group, insurance, and organ transplanted. Races were grouped into white, Black, Hispanic, Asian or other race. The other group includes patients who identified as other, multiracial and those whose race was unavailable. Patients’ primary insurance was grouped into private, Medicare or Medicaid. Significance levels were all set at p < 0.05, two-tailed. Statistical analyses were performed using Stata software, version 15.1 (StataCorp, College Station, TX).
Results
There were 3,001 patients that met criteria for inclusion. Nearly 7% of patients had LEP, and the most commonly preferred language other than English among those patients was Spanish (60%) (data not shown). Just over half of the study population (53%) was vaccinated during the study duration. Median date of vaccination was 29th January 2021, 7 days after notification and 42 days after the first patient in the cohort was vaccinated; presumably the few patients vaccinated prior to notification were part of another eligible group such as healthcare providers. The marked increase in vaccination rate then coincides with notifications (Figure 1).
FIGURE 1
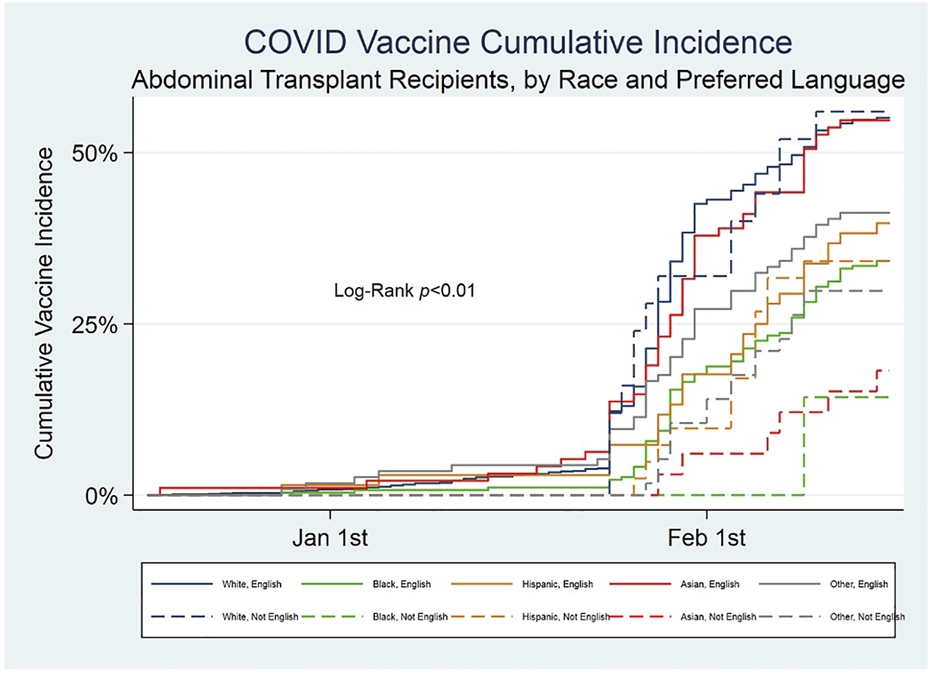
Cumulative incidence of COVID-19 first vaccination among abdominal transplant recipients, by race and preferred language.
On unadjusted analysis, patients not yet vaccinated were significantly more likely to have LEP, be younger, have Medicaid insurance, and identify as a race other than white (Table 1). The cox proportional hazard model of vaccination during the study period demonstrated that patients with a preferred language other than English were less likely to be vaccinated (0.64, p = 0.001) during the study duration, even after adjustment for race (Table 2). Black, Hispanic and other race patients were less likely to be vaccinated compared to the white group (0.58, 0.67, 0.68; all p-value<0.03). When the population is split into groups by race, there is a trend to reduced access among non-white patients with LEP (Figure 2). This is most pronounced in the Black, Asian and other race groups, though the 95% confidence intervals overlap in all but the Asian group. A difference between LEP and EP (English proficient) patients’ likelihood of vaccination was not observed among Hispanic patients.
TABLE 1
| n = 3,001 | Not Vaccinated | Vaccinated | p-value | |
|---|---|---|---|---|
| n = 1,496 | n = 1,505 | |||
| Preferred Language not English | 130 (8.7%) | 63 (4.2%) | <0.001 | |
| Female | 606 (40.5%) | 571 (37.9%) | 0.15 | |
| Race | White | 999 (66.8%) | 1,192 (79.2%) | <0.001 |
| Black | 196 (13.1%) | 113 (7.5%) | ||
| Hispanic | 73 (4.9%) | 42 (2.8%) | ||
| Asian | 88 (5.9%) | 79 (5.2%) | ||
| Other/Multi | 140 (9.4%) | 79 (5.2%) | ||
| Age | <45 | 310 (20.7%) | 211 (14.0%) | <0.001 |
| 45–64 | 669 (44.7%) | 659 (43.8%) | ||
| 65–74 | 389 (26.0%) | 501 (33.3%) | ||
| 75+ | 128 (8.6%) | 134 (8.9%) | ||
| Insurance | Private | 727 (48.6%) | 780 (51.8%) | <0.001 |
| Medicare | 667 (44.6%) | 667 (44.3%) | ||
| Medicaid | 102 (6.8%) | 58 (3.9%) | ||
| Organ | Kidney | 1,100 (73.5%) | 1,120 (74.4%) | 0.81 |
| Liver | 354 (23.7%) | 347 (23.1%) | ||
| Both | 42 (2.8%) | 38 (2.5%) |
Unadjusted comparisons of study population.
TABLE 2
| n = 3,001 | Hazard ratio | p-value | 95% CI | |
|---|---|---|---|---|
| Preferred Language not English | 0.64 | 0.001 | 0.5 to 0.8 | |
| Female | 0.95 | 0.31 | 0.9 to 1.1 | |
| Race | White | Reference | ||
| Black | 0.58 | <0.001 | 0.5 to 0.7 | |
| Hispanic | 0.67 | 0.02 | 0.5 to 0.9 | |
| Asian | 0.93 | 0.57 | 0.7 to 1.2 | |
| Other/Multi | 0.68 | 0.001 | 0.5 to 0.9 | |
| Age | <45 | Reference | ||
| 45–64 | 1.24 | 0.008 | 1.1 to 1.4 | |
| 65–74 | 1.51 | <0.001 | 1.3 to 1.8 | |
| 75+ | 1.3 | 0.02 | 1.0 to 1.6 | |
| Insurance | Private | Reference | ||
| Medicare | 0.87 | 0.02 | 0.8 to 1.0 | |
| Medicaid | 0.76 | 0.05 | 0.6 to 1.0 | |
| Organ | Kidney | Reference | ||
| Liver | 0.91 | 0.15 | 0.8 to 1.0 | |
| Both | 0.87 | 0.42 | 0.6 to 1.2 |
Adjusted regression, likelihood of vaccination during the study time.
FIGURE 2
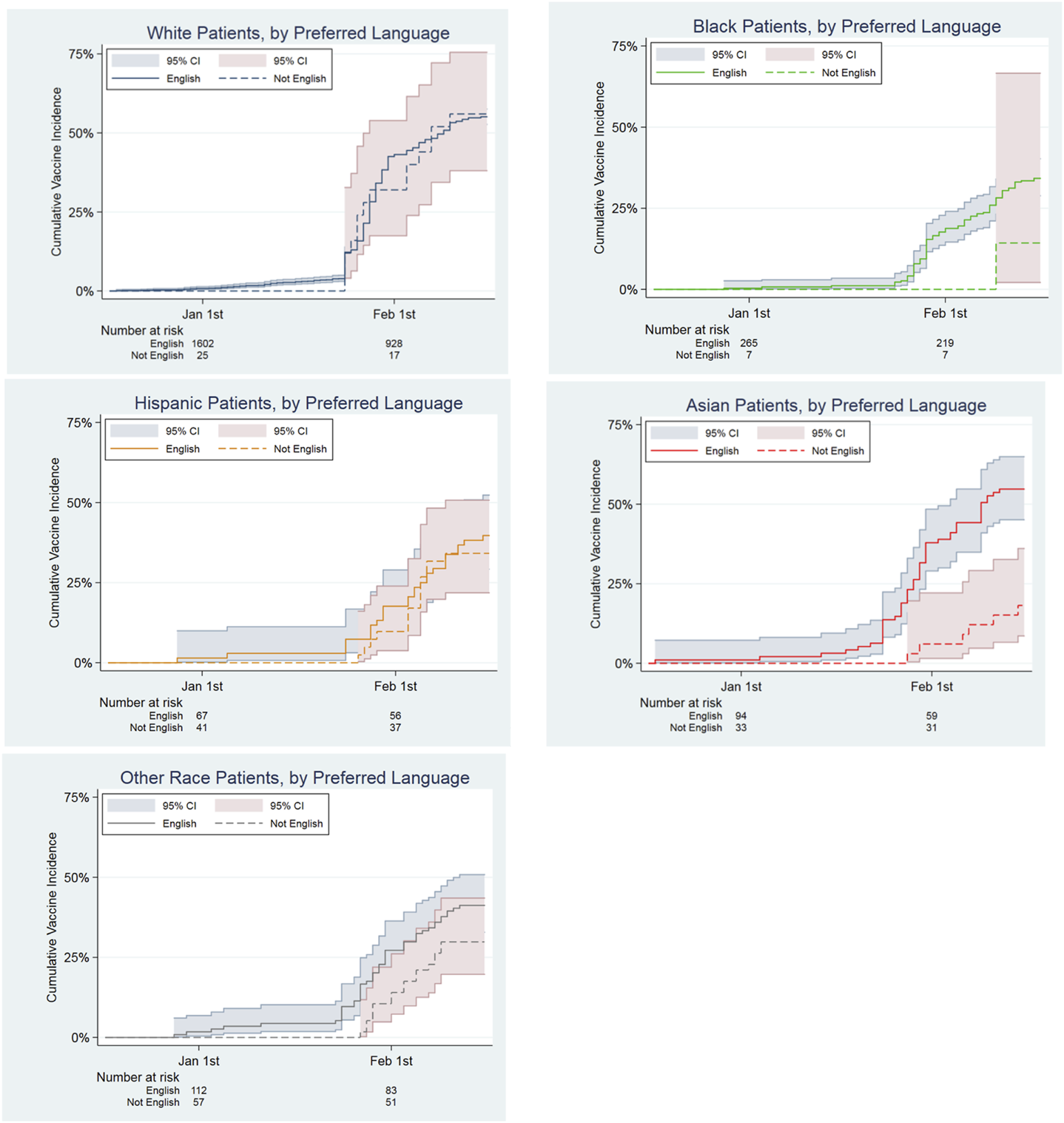
Hazard Ratios of Time to First COVID Vaccination by Race among Abdominal Transplant Recipients, comparing English as Preferred Language to Other Language Preferred.
Discussion
This analysis demonstrates that LEP is an additive barrier to accessing timely COVID vaccination that exacerbates the well-documented disparities related to race. Since at the time of this study vaccines were only available via the medical institution, and this population has established care with this institution, there is less heterogeneity than with community-based vaccination and the general community. Undergoing the process of transplantation and follow-up care can provide a degree of healthcare literacy (10) that further decreases the heterogeneity of social determinants of health in this population. While social determinants of health can be difficult to change, our study suggests a potential intervention by the medical community to address the disparities experienced by patients with LEP. Greater than 95% of the LEP Hispanic patients in this study speak Spanish (data not shown), the authors speculate that the reduced disparity among Hispanic abdominal transplant recipients compared to the other non-white races may reflect the impact from the notice being emailed out in Spanish as well as English. This observation suggests the possibility that language support could ameliorate the impact of racial disparity in this population. The potential impact of language support is further suggested in Asian patients, who did not receive language concordant notices. In that case, Asian patients with LEP were less likely to be vaccinated than EP Asian patients and white patients. This suggests that outreach expanded to provide language concordant communication to these patients could improve timely access to care. Though the number of white patients with LEP was small, there was no difference in time to vaccination compared to white patients who speak English, raising concerns that the disparity related to language proficiency predominantly disadvantages transplant patients who are not white. As prior research has argued, there is an onus on the health system to improve access for these patients in an effort to reduce disparities, with potential methods including patient navigators reaching out with medical interpreters, language concordant communication materials, and involving community organizations to develop outreach to these underserved patients (11). The effects of race and language are likely to be even greater in the general population, compared to the post-transplant population in this study. Vaccine availability has improved in the United States, but remains limited in many areas of the world, and these findings suggest attention to the impact of limited proficiency in the local primary language on access to timely vaccination in global communities. These findings regarding disparities in access to timely care merit broader study to determine if there is an exacerbating impact of language proficiency as an independent barrier to access to other important components of healthcare for patients who do not speak the local majority language. In the meantime, efforts should be expanded to provide patients consistent communication in their preferred language.
Statements
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by MGH Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
CMC participated in research design, writing of the paper, the performance of the research, the data analysis and the interpretation of results. YWC participated in the data analysis and the interpretation of results. DC participated in the data analysis and the interpretation of results. HY participated in research design, access to and interpretation of the data used, the data analysis and the interpretation of results.
Acknowledgments
The authors would like to acknowledge the transplant clinic team for their work assisting and tracking transplant recipients’ COVID vaccinations.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Karliner LS Jacobs EA Chen AH Mutha S . Do professional Interpreters Improve Clinical Care for Patients with Limited English Proficiency? A Systematic Review of the Literature. Health Serv Res (2007) 42(2):727–54. 10.1111/j.1475-6773.2006.00629.x
2.
Biswas S Seman M Cox N Neil C Brennan A Dinh D et al Impact of Limited English Proficiency on Presentation and Outcomes of Patients Undergoing Primary Percutaneous Coronary Intervention for ST-Elevation Myocardial Infarction. Intern Med J (2018) 48(4):457–61. 10.1111/imj.13751
3.
Sentell T Chang A Ahn HJ Miyamura J . Maternal Language and Adverse Birth Outcomes in a Statewide Analysis. Women Health (2016) 56(3):257–80. 10.1080/03630242.2015.1088114
4.
Rozenfeld Y Beam J Maier H Haggerson W Boudreau K Carlson J et al A Model of Disparities: Risk Factors Associated with COVID-19 Infection. Int J Equity Health (2020) 19(1):126. 10.1186/s12939-020-01242-z
5.
Kim HN Lan KF Nkyekyer E Neme S Pierre-Louis M Chew L et al Assessment of Disparities in COVID-19 Testing and Infection across Language Groups in Seattle, Washington. JAMA Netw Open (2020) 3(9):e2021213. 10.1001/jamanetworkopen.2020.21213
6.
Ingraham NE Purcell LN Karam BS Dudley RA Usher MG Warlick CA et al Racial/Ethnic Disparities in Hospital Admissions from COVID-19 and Determining the Impact of Neighborhood Deprivation and Primary Language. medRxiv (2020) 09(2):20185983. 10.1101/2020.09.02.20185983
7.
Diamond LC Jacobs EA Karliner L . Providing Equitable Care to Patients with Limited Dominant Language Proficiency amid the COVID-19 Pandemic. Patient Educ Couns (2020) 103(8):1451–2. 10.1016/j.pec.2020.05.028
8.
Coll E Fernández-Ruiz M Sánchez-Álvarez JE Martinez-Fernandez JR Crespo M Gayoso J et al COVID-19 in Transplant Recipients: The Spanish Experience. Am J Transpl (2021) 21(5):1825–37. 10.1111/ajt.16369
9.
Azzi Y Bartash R Scalea J Loarte-Campos P Akalin E . COVID-19 and Solid Organ Transplantation: A Review Article. Transplantation (2021) 105(1):37–55. 10.1097/TP.0000000000003523
10.
Dahl KG Wahl AK Urstad KH Falk RS Andersen MH . Changes in Health Literacy during the First Year Following a Kidney Transplantation: Using the Health Literacy Questionnaire. Patient Educ Couns (2021) 104(7):1814–22. 10.1016/j.pec.2020.12.028
11.
Fuchs JR Fuchs JW Tietz SE Lum HD . Older Adults with Limited English Proficiency Need Equitable COVID-19 Vaccine Access. J Am Geriatr Soc (2021) 69(4):888–91. 10.1111/jgs.17069
Summary
Keywords
transplant recipients, COVID-19 vaccination, healthcare access, language, disparities
Citation
de Crescenzo CM, Chen Y-W, Chang DC and Yeh H (2023) The Effect of Language on Access to Timely COVID-19 Vaccination of Solid Abdominal Organ Transplant Recipients. Transpl Int 36:10888. doi: 10.3389/ti.2023.10888
Received
05 September 2022
Accepted
31 January 2023
Published
14 February 2023
Volume
36 - 2023
Updates
Copyright
© 2023 de Crescenzo, Chen, Chang and Yeh.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Heidi Yeh, hyeh@mgh.harvard.edu
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.