Abstract
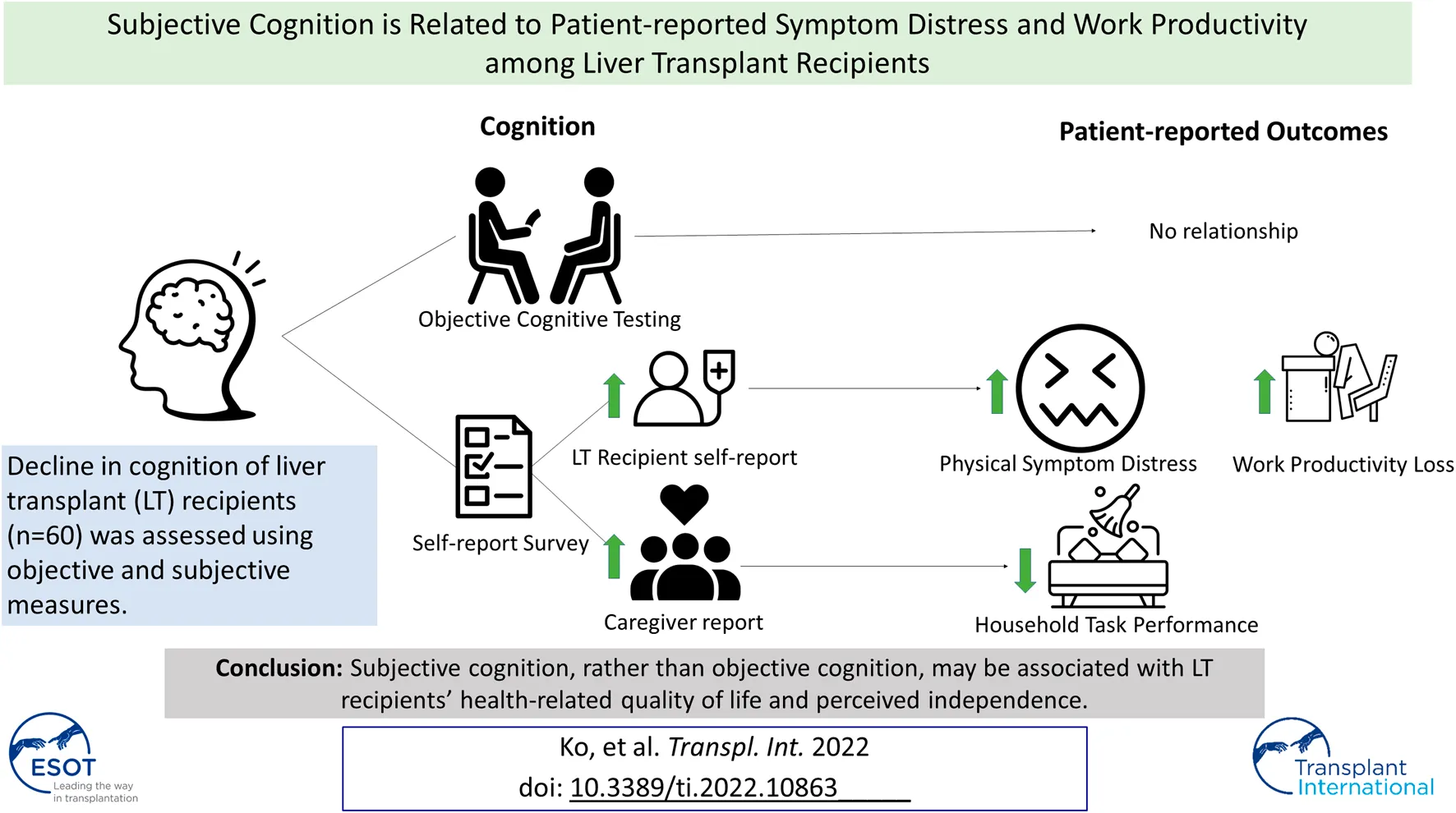
Cognitive decline may prevent liver transplant (LT) recipients from staying healthy and independent. This study examined associations of objective and subjective, rated by LT recipients and caregivers, cognitive decline with patient-reported physical and psychological symptom distress, ability to perform household tasks, and workplace productivity among LT recipients. Sixty pairs of LT recipients and caregivers participated in this cross-sectional study. Subjective cognition was measured by the Everyday Cognition. Objective cognition was assessed with four cognitive tests, including the Repeatable Battery for the Assessment of Neuropsychological Status. Patient-reported outcomes were assessed with the Rotterdam Symptom Checklist-Modified, Profile of Mood States-Short Form, Creative Therapy Consultants Homemaking Assessment, and Work Limitations Questionnaire. Linear regression analyses related objective and subjective cognition to the patient-reported outcomes. While objective cognitive decline was not associated with any patient-reported outcomes, subjective cognitive decline was significantly associated with the outcomes. Higher LT recipient self-rated cognitive decline was associated with higher physical symptom distress ( = 0.30, p = 0.006) and workplace productivity loss ( = 14.85, p < 0.0001). Higher caregiver-rated cognitive decline was associated with lower household tasks performance ( = −18.55, p = 0.015). Findings suggest to consider subjective cognition when developing an individualized post-transplant care plan.
Introduction
As more than 80% of liver transplant (LT) recipients survive beyond 5 years post-transplant (1), maintaining healthy and independent lives has become one of the top priorities for post-LT care (2). While some LT recipients tend to carry out activities to stay healthy and independent after LT, such as taking medication as prescribed or returning to employment, others do not. Up to 75% of LT recipients are non-adherent to their medication regimen (3–5), and less than 60% engage in either non-paid (e.g., homemakers or students) or paid work (6). Cognitive decline could be one of the potential factors that prevent successful performance of such activities. In fact, 9%–56% of LT recipients have objective impairment on formal cognitive testing (7–9).
Cognitive health is an important consideration for post-transplant recipients as cognitive decline after LT may affect recipients’ abilities to maintain healthy and independent lives. Intact cognition, particularly in memory, attention, and executive function, is required for successful performance of tasks necessary to maintaining overall health and independence (10). For example, LT recipients should perform health maintenance tasks, such as monitoring and managing symptoms and side effects of immunosuppressants. However, recipients with cognitive decline in the above areas may have reduced abilities to monitor and manage symptoms (11, 12) that potentially lead to physical and psychological symptom distress. Furthermore, decline in cognition, including the aforementioned domains, may reduce work capacity and productivity (13, 14). Recipients with cognitive decline may not be able to successfully perform household tasks, return to work, or stay employed after LT. While cognitive health appears to relate to physical and psychological symptom distress, ability to perform household tasks, and workplace productivity, there is a paucity of literature examining these associations. Understanding cognitive decline in relation to these patient-reported outcomes may expand our knowledge regarding overall wellbeing and disease burden associated with cognitive decline in this population. Further, such knowledge may also inform how clinicians can facilitate LT recipients in achieving healthy and independent lives.
This study investigated the associations between cognition and patient-reported outcomes of physical and psychological symptom distress, ability to perform household tasks, and workplace productivity among LT recipients. Objective and subjective measures of cognition (global and multiple specific domains) were assessed in relation to the patient-reported outcomes. We included subjective cognitive measures, reported by LT recipients and caregivers, to assess the feasibility of using these self-report cognitive measures given the ease of use in clinical practice (15). We included caregivers in this study since caregivers may estimate LT recipients’ cognition differently than recipients themselves (15). Subjective cognition reported by LT recipients and caregivers could be variously associated with patient-reported outcomes. In this study, caregivers were queried about perceived LT recipients’ cognition. We hypothesized that LT recipients with worse objective cognitive test scores or greater subjective cognitive decline reported by LT recipients or caregivers have worse symptom distress, poorer ability to perform household tasks, and decreased workplace productivity than those with better objective cognitive test scores or subjective cognitive status. This study further examined whether the above associations differ by post-transplant employment status because employment affects cognition (16).
Patients and Methods
Population
A convenience sampling was used in this cross-sectional single center study to recruit participants between December 2018 and September 2019. LT recipients were eligible to participate in this study if they were over 18 years old, had received a LT at least more than 3 months ago (to minimize the potential influences of early post-operative complications) but not more than 2 years post-transplant, had caregivers who could answer questions about the recipients’ cognition, and were able to speak and write English. LT recipients were excluded from this study if they had received any other organ transplant, such as kidney, had a history of a neurological disorder, such as Alzheimer’s disease or stroke, had a history of head injury, or were not able to provide informed consent. Caregivers identified by participating LT recipients were included in this study if they were over 18 years old and able to speak and write English. Those who were not able to provide informed consent were excluded from this study. Recruitment process of participants are described elsewhere (15), but in short, a total of 207 LT recipients were invited to participate in the study, and 60 provided written informed consent.
Measures
LT recipients completed an online self-report survey assessing subjective cognition and patient-reported outcomes of physical and psychological symptom distress, ability to perform household tasks, and workplace productivity via Research Electronic Data Capture (REDCap) (17, 18). They then completed in-person, paper-and-pencil objective cognitive tests. Caregivers completed an online self-report survey assessing subjective cognition via REDCap.
Cognition
Subjective Cognition
The 39-item Modified Everyday Cognition (ECog) was used to assess LT recipient self-rated and caregiver-rated cognition in six domains: memory, language, visuospatial abilities, planning, organization, and divided attention (19, 20). LT recipients rated their current perceived difficulties in performing daily activities, and caregivers rated perceived difficulties that LT recipients currently have in performing daily activities from 1 (no difficulty) to 4 (severe difficulty/cannot do). “Don’t know” was available and scored as 0. Mean total scores that represent global subjective cognition and mean domain scores are available with higher scores indicating greater perceived difficulties in performing daily activities (19). The ECog was found to be valid in differentiating cognitive decline from normal cognition (19). Cronbach’s alpha coefficients in this study sample were good (0.89–0.98).
Objective Cognition
Global cognition was measured by the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) (21). The RBANS assesses five domains, attention, language, visuospatial/constructional abilities, and immediate and delayed memory, with 12 tests. Higher total scores indicate better global cognition (21). The RBANS has been shown to be effective in detecting mild cognitive impairment (22).
Cognition in three domains most commonly found to be impaired in the LT population (visuospatial abilities, executive function, and attention) (7, 23) were additionally assessed using reliable and valid cognitive tests. The Trail Making Test Parts A and B assess attention and executive function, respectively, and longer total time to complete the test indicates worse cognition (24). The Digit Span Backward test from the Neuropsychological Assessment Battery (NAB) assesses attention and executive function, and higher total scores are indicative of better cognition (25). The Rey-Osterrieth Complex Figure (Copy) assesses visuospatial constructional ability and executive function, and higher total scores are indicative of better cognition (26–28).
Patient-Reported Outcomes
Symptom Distress
The 28-item Rotterdam Symptom Checklist-Modified (RSCL-M) (29) asked LT recipients to rate the extent of physical symptom distress in the past week from 1 (Not at all) to 4 (Very much). Higher mean total scores indicate worse physical symptom distress (29). The validity of this questionnaire has been previously established (29). Cronbach’s alpha of this questionnaire was 0.89 in the current study. The 37-item Profile of Mood States-Short Form (POMS-SF) (30) asked LT recipients to rate their psychological distress in six subscales (depression, vigor, confusion, tension, anger, and fatigue) in the past 2 weeks from 0 (Not at all) to 4 (Extremely). Higher mean total scores indicate worse psychological distress (30). The validity of POMS-SF was established in various populations, including the kidney transplant population (30). Cronbach’s alpha of this questionnaire ranged from 0.82 to 0.95 in this study.
Ability to Perform Household Tasks
LT recipients completed the Creative Therapy Consultants (CTC) Homemaking Assessment, which was found to be reliable and valid to assess the performance of 29 household tasks in three categories: light (e.g., folding clothes), medium (e.g., washing dishes), and heavy (e.g., grocery shopping) tasks (31). Participants rated how much assistance they need to complete the tasks from 0 (Cannot complete without assistance) to 1 (Complete with no assistance). “Not applicable” was available if participants do not engage in certain tasks and scored as 0. Higher total weighted scores indicate higher household work productivity (32). Cronbach’s alpha for this questionnaire ranged between 0.84 and 0.92 in this study.
Workplace Productivity
LT recipients who were employed full-time or part-time at the time of survey administration completed the 25-item Work Limitations Questionnaire (WLQ) (33, 34). This questionnaire assesses the interference of health conditions in workplace productivity in four scales: Time, Physical, Mental-Interpersonal, and Output Demands. Participants rated difficulties at work in the past 2 weeks from 1 (None of the time) to 5 (All of the time) and rated their ability to work in the past 2 weeks from 1 (Able all of the time) to 5 (Able none of the time). “Does not apply to my job” was also available scoring as 0. Higher total scores indicate higher self-reported at-work productivity loss in the past 2 weeks (35). The WLQ has been validated with chronic disease populations (34). Cronbach’s alpha for this questionnaire ranged from 0.79 to 0.96 in this study.
Demographic and Clinical Characteristics
LT recipients and caregivers completed a self-report demographic questionnaire. Clinical characteristics of LT recipients, such as the date of transplant and Model for End Stage Liver Disease-Sodium (MELD) score (36), were extracted from medical records.
Analysis
IBM SPSS Statistics version 26 (IBM, Armonk, NY, United States) and SAS Version 9.4 (SAS Institute, Cary, NC) were used to perform data analysis. Patient characteristics and scores for the study measures were described using means and standard deviations (SDs) for continuous measures and counts and proportions for categorical variables. Unadjusted and adjusted linear regression models were developed to examine the relationships of subjective and objective cognitive test scores with physical and psychological symptom distress and household tasks performance; adjusted models included LT recipients’ age, education, and months since LT. Only an unadjusted regression model was reported for workplace productivity due to the small number of subjects who were working either full- or part-time at the time of survey administration (n = 17). Among the four objective cognitive tests, only the RBANS that indicates global cognition was included in the models given the small sample size. For all models, the coefficient estimates were tabulated along with 95% confidence intervals (CI) and p-values. Correlations between subjective and objective cognitive domain scores and patient-reported outcomes were examined using Pearson’s correlation coefficient with 95% CIs to investigate which domains were specifically correlated with the outcomes. A two-tailed alpha of 0.05 was set as the level of statistical significance. Listwise deletion was used to deal with missing data.
This study performed additional analyses to examine differences in the findings by post-transplant employment status. Independent group t-tests, assuming unequal variance, were used to compare subjective and objective cognitive test scores and patient-reported outcomes of physical and psychological symptom distress and household tasks performance between employed and non-employed LT recipients. Unadjusted regression analyses and Pearson’s correlation coefficients, comparing the same variables as above but stratified by post-transplant employment status, were also performed.
Results
Participant Characteristics
Sixty pairs of LT recipients and their caregivers participated in this study. Table 1 summarizes the demographic of LT recipients. Most LT recipients were male (71.7%), white (93.3%), and married (71.7%). They had a mean age of 60.4 (SD = 6.9) and a mean of 14.1 (SD = 2.4) years of education, and mean time elapsed since LT was 12.9 months (SD = 7.0). The most common cause of liver failure was Non-alcoholic steatohepatitis (46.7%), and mean MELD score at LT was 21.7 (SD = 10.0; Table 1).
TABLE 1
| Characteristics | Frequency (%) or mean (SD) | ||
|---|---|---|---|
| All LT recipients (N = 60) | LT recipients Employed (N = 17) | LT Recipients Not Employed (N = 43) | |
| Age (years) | 60.4 (6.9) | 57.9 (5.9) | 61.5 (7.0) |
| Sex | |||
| Male | 43 (71.7%) | 12 (70.6%) | 31 (72.1%) |
| Female | 17 (28.3%) | 5 (29.4%) | 12 (27.9%) |
| Race | |||
| Black | 2 (3.3%) | 0 (0.0%) | 2 (4.7%) |
| White | 56 (93.3%) | 16 (94.1%) | 40 (93.0%) |
| Other (e.g., aboriginal) | 2 (3.3%) | 1 (5.9%) | 1 (2.3%) |
| Marital Status | |||
| Single | 10 (16.7%) | 2 (11.8%) | 8 (18.6%) |
| Single, living with partner | 3 (5.0%) | 2 (11.8%) | 1 (2.3%) |
| Married | 43 (71.7%) | 12 (70.6%) | 31 (72.1%) |
| Widowed/separated | 4 (6.7%) | 1 (5.9%) | 3 (7.0%) |
| Education | 14.1 (2.4) | 14.5 (3.0) | 13.9 (2.1) |
| Household income | |||
| $20,000 or less | 10 (20.0%) | 0 (0.0%) | 10 (27.7%) |
| $20,001 to $40,000 | 9 (18.0%) | 1 (7.1%) | 8 (22.2%) |
| $40,001 to $60,000 | 10 (20.0%) | 2 (14.2%) | 8 (22.2%) |
| Over $60,000 | 21 (42.0%) | 11 (78.6%) | 10 (27.8%) |
| Insurance | |||
| Government insurance | 23 (38.3%) | 2 (11.8%) | 21 (48.8%) |
| Non-government insurance | 32 (53.3%) | 13 (76.5%) | 19 (44.2%) |
| Multiple | 4 (6.7%) | 1 (5.9%) | 3 (7.0%) |
| None | 1 (1.7%) | 1 (5.9%) | 0 (0.0%) |
| Cause of liver disease | |||
| Non-alcoholic steatohepatitis | 28 (46.7%) | 6 (35.3%) | 22 (51.2%) |
| Alcohol | 10 (16.7%) | 2 (11.8%) | 8 (18.6%) |
| Hepatitis C | 11 (18.3%) | 5 (29.4%) | 6 (14.0%) |
| Autoimmune/cholestatic | 7 (11.7%) | 3 (17.6%) | 4 (9.3%) |
| Others | 4 (6.7%) | 1 (5.9%) | 3 (7.0%) |
| History of pre-transplant hepatic encephalopathy | |||
| No | 17 (28.3%) | 9 (52.9%) | 8 (18.6%) |
| Yes | 43 (71.7%) | 8 (47.1%) | 35 (81.4%) |
| Time since transplant (months) | 12.9 (7.0) | 11.8 (6.8) | 13.4 (7.1) |
| MELD score | 21.7 (10.0) | 13.6 (6.0) | 24.9 (9.4) |
Participant characteristics.
Seventeen of 60 LT recipients were employed full time (n = 15, 25.0%) or part time (n = 2, 3.3%) after LT. While the characteristics of employed were generally comparable to non-employed LT recipients, employed recipients were relatively younger (mean age = 57.9, SD = 5.9 versus mean age = 61.5, SD = 7.0) and had a higher annual household income (annual household income over $60,000: 78.6% versus 27.8%). A smaller number of employed recipients had pre-transplant hepatic encephalopathy (47.1% versus 81.4%) and they had a lower MELD score at LT than the non-employed recipients (mean = 13.6, SD = 6.0 versus mean = 24.9, SD = 9.4; Table 1).
Most caregivers participated in this study were the spouse or significant other (73.3%) of LT recipients with a mean of 35 (SD = 12.6) years length of relationship. They tended to be female (80.0%), white (94.9%), and had a mean age of 57.1 (SD = 11.8) years and a mean of 13.9 (SD = 2.1) years of education. They reported that they spend a mean of 107 (SD = 56.8) hours per week with LT recipients.
Subjective and Objective Cognition
The ECog scores of LT recipients are summarized in Table 2. Summaries of caregivers’ ECog scores were reported elsewhere (15) but briefly, scores of both LT recipients’ and caregivers’ ECog indicate mild perceived difficulties in performing daily activities (mean = 1.5, SD = 0.5; mean = 1.4, SD = 0.5).
TABLE 2
| All LT recipients (N = 60) | LT recipients employed (N = 17) | LT recipients not employed (N = 43) | p-valuea | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Ecog | ||||
| Global | 1.5 (0.5) | 1.2 (0.3) | 1.6 (0.5) | 0.002 |
| Memory | 1.7 (0.5) | 1.4 (0.4) | 1.8 (0.5) | 0.004 |
| Language | 1.5 (0.6) | 1.2 (0.3) | 1.6 (0.6) | 0.004 |
| Visuospatial abilities | 1.2 (0.4) | 1.0 (0.1) | 1.3 (0.5) | 0.000 |
| Planning | 1.3 (0.5) | 1.2 (0.3) | 1.4 (0.5) | 0.076 |
| Organization | 1.5 (0.7) | 1.2 (0.3) | 1.7 (0.7) | 0.001 |
| Divided attention | 1.5 (0.7) | 1.4 (0.6) | 1.6 (0.7) | 0.290 |
| RBANSb | ||||
| Global | 194.0 (25.5)c | 210.9 (14.7)d | 187.5 (25.9)e | <0.0001 |
| Immediate memory index | 40.1 (7.7)c | 44.8 (5.0)d | 39.3 (8.1)e | 0.003 |
| Visuospatial/constructional index | 31.1 (4.5)c | 32.3 (3.3)d | 30.7 (4.8)e | 0.154 |
| Language index | 28.6 (4.5)c | 29.7 (4.6)d | 28.1 (4.4)e | 0.251 |
| Attention index | 48.9 (11.5)c | 56.4 (6.8)d | 46.0 (11.7)e | 0.000 |
| Delayed memory index | 44.6 (5.7)c | 47.6 (4.1)d | 43.4 (5.9)e | 0.004 |
| Trail Making Test | ||||
| Part A | 35.8 (17.1)c | 29.1 (7.4)d | 38.4 (19.1)e | 0.010 |
| Part B | 90.0 (45.8)c | 67.0 (16.5)d | 98.9 (50.4)e | 0.001 |
| NAB Digit Span Backward | 4.2 (2.0)c | 4.9 (1.5)d | 4.0 (2.0)e | 0.071 |
| Rey-Osterrieth Complex Figure (Copy) | 27.6 (4.9)c | 29.8 (4.3)d | 26.7 (4.9)e | 0.025 |
| RSCL-M | 1.6 (0.4)c | 1.6 (0.5)d | 1.6 (0.3)e | 0.833 |
| POMS-SF | ||||
| Total score | 0.8 (0.5) | 0.9 (0.5) | 0.8 (0.5) | 0.527 |
| Depression | 0.5 (0.7) | 0.5 (0.7) | 0.5 (0.7) | 0.920 |
| Vigor | 1.6 (1.0) | 1.9 (1.0) | 1.6 (1.0) | 0.289 |
| Confusion | 0.6 (0.6) | 0.4 (0.6) | 0.7 (0.6) | 0.209 |
| Tension | 0.6 (0.7) | 0.7 (0.7) | 0.6 (0.7) | 0.687 |
| Anger | 0.5 (0.6) | 0.6 (0.6) | 0.4 (0.6) | 0.240 |
| Fatigue | 1.0 (1.0) | 1.2 (1.1) | 1.0 (0.9) | 0.505 |
| CTC Homemaking Assessment | 90.5 (21.6)f | 97.3 (7.9) | 87.5 (24.9)g | 0.031 |
| WLQ | ||||
| Total Productivity Loss Score | 3.4 (4.8)d | |||
| Time Scale | 17.0 (26.3)d | |||
| Physical Scale | 16.9 (24.1)d | |||
| Mental-Interpersonal Scale | 8.0 (14.2)d | |||
| Output Scale | 12.8 (21.5)d | |||
Summary of subjective and objective cognition, symptom distress, household tasks performance, and workplace productivity.
Note: Bold values denote statistical significance at the p < 0.05 level.
aComparisons of cognition, symptom distress, household tasks performance, and workplace productivity between employed and non-employed LT recipients.
bScores presented as raw scores.
cn = 57.
n = 16.
n = 41.
n = 56.
n = 39.
See Table 2 for the summary of objective cognitive performance.
Cognition and Post-Transplant Employment Status
Compared to LT recipients who did not return to work, employed LT recipients had lower global ECog scores (indicating less subjective concerns about cognition) and higher scores on global objective cognition and multiple domains (indicating higher levels of objective cognition; Table 2).
Patient-Reported Outcomes
Summaries of patient-reported outcomes are described in Table 2. Scores of the RSCL-M and the POMS-SF indicated that LT recipients in this study have mild physical (mean = 1.6, SD = 0.4) and psychological symptom distress (mean = 0.8, SD = 0.5). Scores of the CTC Homemaking Assessment indicate that LT recipients could perform approximately 90% (SD = 21.6) of household tasks (Table 2).
Patient-Reported Outcomes and Post-Transplant Employment Status
LT recipients who returned to work after LT reported that they experience 3.4% (SD = 4.8) of productivity loss at work (Table 2). While the time scale score was the highest (mean = 17.0, SD = 26.3) indicating that recipients perceive the greatest difficulties handling time and scheduling demands at work, the mental-interpersonal scale score was the lowest (mean = 8.0, SD = 14.2) indicating that recipients perceive the lowest difficulties when performing tasks that require cognitive or social skills at work. Employed LT recipients had higher CTC Homemaking Assessment scores than non-employed recipients, while no significant differences were found in RCSL-M and POMS-SF scores (Table 2).
Associations Between Subjective Cognition and Patient-Reported Outcomes
Higher total ECog scores of LT recipients were significantly associated with higher RSCL-M scores ( = 0.30, p = 0.006; Table 3). Domain analysis revealed that ECog scores in all domains except for visuospatial abilities were fair to moderately associated with RSCL-M scores (r = 0.40–0.58; Table 4). Higher total ECog scores of caregivers were significantly associated with lower CTC Homemaking Assessment scores ( = −18.55, p = 0.015; Table 3). Specifically, their ECog scores in memory and language were negatively correlated to CTC scores (r = −0.28 and −0.34, respectively; Table 4).
TABLE 3
| Unadjusted | Adjusteda | |||||
|---|---|---|---|---|---|---|
| N | (95% CI) | p-value | N | (95% CI) | p-value | |
| RSCL-M | ||||||
| LT recipient ECog | 60 | 0.39 (0.22, 0.57) | <0.0001 | 54 | 0.30 (0.09, 0.51) | 0.006 |
| Caregiver ECog | 60 | 0.29 (0.10, 0.48) | 0.004 | 0.14 (−0.08, 0.36) | 0.213 | |
| LT recipient RBANS | 57 | −0.00 (−0.01, 0.00) | 0.172 | 0.00 (−0.00, 0.01) | 0.661 | |
| POMS-SF | ||||||
| LT recipient ECog | 60 | 0.27 (0.02, 0.52) | 0.035 | 54 | 0.25 (−0.04, 0.55) | 0.091 |
| Caregiver ECog | 60 | 0.27 (0.01, 0.52) | 0.040 | 0.18 (−0.13, 0.49) | 0.245 | |
| LT recipient RBANS | 57 | 0.00 (−0.00, 0.01) | 0.255 | 0.00 (−0.00, 0.01) | 0.210 | |
| CTC Homemaking Assessment | ||||||
| LT recipient ECog | 56 | −7.34 (−19.20, 4.51) | 0.220 | 50 | 2.09 (−12.54, 16.71) | 0.775 |
| Caregiver ECog | 56 | −13.24 (−24.89, −1.60) | 0.027 | −18.55 (−33.38, −3.73) | 0.015 | |
| LT recipient RBANS | 53 | 0.01 (−0.24, 0.27) | 0.916 | −0.26 (−0.55, 0.04) | 0.090 | |
| WLQb | ||||||
| LT recipient ECog | 16 | 14.85 (10.40, 19.30) | <0.0001 | |||
| Caregiver ECog | 16 | 4.92 (−3.09, 12.94) | 0.209 | |||
| LT recipient RBANS | 15 | −0.13 (−0.31, 0.05) | 0.129 | |||
Associations between subjective and objective cognition and symptom distress, household tasks performance, and workplace productivity.
Note: Bold values denote statistical significance at the p < 0.05 level.
Adjusted for LT recipients’ age, education, and months since transplant.
Adjusted model for workplace productivity was not possible due to the small sample size (n = 16).
TABLE 4
| RSCL-M | POMS-SF | CTC homemaking assessment | WLQa | ||||||
|---|---|---|---|---|---|---|---|---|---|
| r (95% CI) | p-value | r (95% CI) | p-value | r (95% CI) | p-value | r (95% CI) | p-value | ||
| LT recipient ECog (n = 60) | Memory | 0.58 (0.38, 0.72) | <0.0001 | 0.31 (0.06, 0.53) | 0.014 | −0.28b (−0.51, −0.02) | 0.032 | 0.86 (0.63, 0.95) | <0.0001 |
| Language | 0.40 (0.17, 0.60) | 0.001 | 0.10 (−0.16, 0.34) | 0.452 | −0.21b (−0.45, 0.06) | 0.123 | 0.68 (0.28, 0.88) | 0.002 | |
| Visuospatial abilities | 0.17 (−0.09, 0.40) | 0.203 | 0.02 (−0.24, 0.27) | 0.879 | −0.00b (−0.27, 0.26) | 0.977 | 0.11 (−0.41, 0.57) | 0.688 | |
| Planning | 0.48 (0.25, 0.65) | <0.0001 | 0.34 (0.09, 0.55) | 0.007 | −0.04b (−0.30, 0.22) | 0.742 | 0.83 (0.56, 0.94) | <0.0001 | |
| Organization | 0.45 (0.22, 0.63) | 0.0002 | 0.31 (0.06, 0.52) | 0.015 | −0.05b (−0.31, 0.22) | 0.730 | 0.66 (0.24, 0.87) | 0.004 | |
| Divided attention | 0.50 (0.28, 0.67) | <0.0001 | 0.39 (0.15, 0.59) | 0.002 | −0.19b (−0.43, 0.08) | 0.168 | 0.87 (0.66, 0.96) | <0.0001 | |
| Caregiver ECog (n = 60) | Memory | 0.42 (0.18, 0.61) | 0.001 | 0.25 (0.00, 0.48) | 0.050 | −0.28b (−0.51, −0.02) | 0.033 | 0.19 (−0.34, 0.63) | 0.469 |
| Language | 0.33 (0.09, 0.54) | 0.008 | 0.15 (−0.11, 0.39) | 0.240 | −0.34b (−0.55, −0.08) | 0.010 | 0.31 (−0.22, 0.70) | 0.228 | |
| Visuospatial abilities | 0.11c (−0.16, 0.36) | 0.435 | 0.10c (−0.17, 0.35) | 0.474 | −0.17d (−0.42, 0.11) | 0.230 | 0.29 (−0.24, 0.69) | 0.267 | |
| Planning | 0.28e (0.02, 0.50) | 0.034 | 0.30e (0.04, 0.52) | 0.022 | −0.22f (−0.46, 0.05) | 0.103 | 0.26 (−0.27, 0.67) | 0.312 | |
| Organization | 0.31g (0.04, 0.54) | 0.023 | 0.22g (−0.06, 0.46) | 0.115 | −0.26h (−0.50, 0.02) | 0.064 | 0.33 (−0.24, 0.73) | 0.233 | |
| Divided attention | 0.38e (0.14, 0.58) | 0.003 | 0.35e (0.10, 0.55) | 0.007 | −0.26f (−0.50, 0.01) | 0.053 | 0.40 (−0.12, 0.75) | 0.112 | |
Correlations between the domains of subjective cognition and symptom distress, household tasks performance, and workplace productivity.
Note: Bold values denote statistical significance at the p < 0.05 level.
an = 16.
n = 56.
n = 55.
n = 53.
n = 58.
n = 54.
n = 52.
n = 50.
Higher LT recipients’ total ECog scores were significantly associated with higher WLQ scores ( = 14.85, p < 0.0001; Table 3). Particularly, ECog scores in the domains of memory, language, planning, organization, and divided attention were correlated with higher scores on the WLQ (r = 0.66–0.87; Table 4). Caregiver ECog scores were not related to the WLQ, regardless of domain (Tables 3, 4). Note, these associations were unadjusted for LT recipients’ age, education, and months since transplant due to a small sample size.
Associations Between Subjective Cognition and Patient-Reported Outcomes by Post-Transplant Employment Status
This study further examined unadjusted associations between subjective cognition and patient-reported outcomes stratified by post-transplant employment status (Tables 5, 6). In the employed group, higher LT recipient total ECog scores were associated with higher RSCL-M ( = 1.05, p = 0.005) and POMS-SF ( = 1.46, p = 0.0003; Table 5). Domain analysis revealed that higher ECog scores of LT recipient in the domains of memory, planning, organization, and divided attention moderately to strongly correlated with higher RSCL-M (r = 0.47–0.69) and POMS-SF (r = 0.50–0.83; Table 6). Higher total ECog scores of both LT recipient and caregiver were related to lower CTC scores ( = −14.96, p = 0.028; = −14.97, p = 0.009, respectively; Table 5). While LT recipient ECog scores in memory and divided attention were related to lower CTC scores (r = −0.50 and −0.77, respectively), all caregiver ECog domain scores except for memory were moderately correlated with CTC Homemaking Assessment scores (r = −0.58–−0.66; Table 6). In the unemployed group, higher LT recipient and caregiver total ECog scores were associated with higher RSCL-M scores ( = 0.36, p = 0.0002; = 0.35, p = 0.0003, respectively). Nearly all of the recipient and caregiver ECog domain scores, except visuospatial abilities, were fair to moderately correlated with higher RSCL-M scores (r = 0.44–0.58 in LT recipients and r = 0.41–0.60 in caregivers; Table 6). No statistically significant associations were noted with POMS-SF or CTC scores (Table 5).
TABLE 5
| LT recipients employed | LT recipients not employed | |||||
|---|---|---|---|---|---|---|
| N | (95% CI) | p-value | N | (95% CI) | p-value | |
| RSCL-M | ||||||
| LT recipient ECog | 17 | 1.05 (0.37, 1.73) | 0.005 | 43 | 0.36 (0.18, 0.54) | 0.0002 |
| Caregiver ECog | 17 | −0.04 (−0.82, 0.74) | 0.917 | 43 | 0.35 (0.17, 0.53) | 0.0003 |
| LT recipient RBANS | 16 | −0.02 (−0.03, −0.00) | 0.018 | 41 | −0.00 (−0.01, 0.00) | 0.504 |
| POMS-SF | ||||||
| LT recipient ECog | 17 | 1.46 (0.80, 2.11) | 0.000 | 43 | 0.20 (−0.07, 0.48) | 0.140 |
| Caregiver ECog | 17 | 0.55 (−0.29, 1.40) | 0.184 | 43 | 0.27 (−0.00, 0.54) | 0.052 |
| LT recipient RBANS | 16 | −0.01 (−0.03, 0.01) | 0.177 | 41 | 0.00 (−0.00, 0.01) | 0.133 |
| CTC Homemaking Assessment | ||||||
| LT recipient ECog | 17 | −14.96 (−28.06, −1.86) | 0.028 | 39 | −3.31 (−19.26, 12.63) | 0.676 |
| Caregiver ECog | 17 | −14.97 (−25.64, −4.30) | 0.009 | 39 | −11.15 (−26.50, 7.20) | 0.150 |
| LT recipient RBANS | 16 | 0.07 (−0.24, 0.38) | 0.642 | 37 | −0.09 (−0.44, 0.25) | 0.588 |
Unadjusted associations between subjective and objective cognition and symptom distress, household tasks performance, and workplace productivity stratified by post-transplant employment status.
Note: Bold values denote statistical significance at the p < 0.05 level.
TABLE 6
| RSCL-M | POMS-SF | CTC homemaking assessment | |||||
|---|---|---|---|---|---|---|---|
| r (95% CI) | p-value | r (95% CI) | p-value | r (95% CI) | p-value | ||
| Employed (n = 17) | |||||||
| LT recipient ECog | Memory | 0.69 (0.32, 0.88) | 0.001 | 0.74 (0.40, 0.90) | 0.0003 | −0.50 (−0.79, −0.02) | 0.035 |
| Language | 0.47 (−0.02, 0.77) | 0.052 | 0.51 (0.04, 0.80) | 0.029 | −0.27 (−0.67, 0.24) | 0.277 | |
| Visuospatial abilities | 0.04 (−0.45, 0.51) | 0.876 | 0.16 (−0.35, 0.60) | 0.528 | −0.09 (−0.54, 0.41) | 0.739 | |
| Planning | 0.63 (0.22, 0.85) | 0.004 | 0.77 (0.46, 0.91) | <0.0001 | −0.41 (−0.74, 0.09) | 0.094 | |
| Organization | 0.54 (0.08, 0.81) | 0.021 | 0.50 (0.03, 0.79) | 0.035 | −0.29 (−0.67, 0.23) | 0.257 | |
| Divided attention | 0.47 (0.01, 0.78) | 0.048 | 0.83 (0.58, 0.94) | <0.0001 | −0.77 (−0.91, −0.47) | <0.0001 | |
| Caregiver ECog | Memory | −0.02 (−0.50, 0.46) | 0.933 | 0.21 (−0.30, 0.63) | 0.404 | −0.37 (−0.72, 0.14) | 0.139 |
| Language | −0.05 (−0.52, 0.44) | 0.840 | 0.30 (−0.22, 0.68) | 0.240 | −0.60 (−0.84, −0.16) | 0.008 | |
| Visuospatial abilities | −0.10 (−0.56, 0.40) | 0.693 | 0.23 (−0.28, 0.64) | 0.372 | −0.61 (−0.84, −0.18) | 0.006 | |
| Planning | −0.08 (−0.54, 0.41) | 0.748 | 0.32 (−0.19, 0.70) | 0.197 | −0.58 (−0.83, −0.14) | 0.011 | |
| Organization | 0.08a (−0.45, 0.57) | 0.771 | 0.33a (−0.22, 0.72) | 0.215 | −0.58a (−0.84, −0.10) | 0.018 | |
| Divided attention | −0.05 (−0.52, 0.44) | 0.849 | 0.41 (−0.09, 0.74) | 0.095 | −0.66 (−0.87, −0.26) | 0.002 | |
| Non-employed (n = 43) | |||||||
| LT recipient ECog | Memory | 0.58 (0.34, 0.75) | <0.0001 | 0.24 (−0.06, 0.51) | 0.115 | −0.21b (−0.49, 0.12) | 0.204 |
| Language | 0.44 (0.16, 0.66) | 0.002 | 0.06 (−0.25, 0.35) | 0.711 | −0.14b (−0.44, 0.18) | 0.378 | |
| Visuospatial abilities | 0.21 (−0.10, 0.48) | 0.173 | 0.05 (−0.25, 0.35) | 0.748 | 0.08b (−0.24, 0.39) | 0.611 | |
| Planning | 0.46 (0.19, 0.67) | 0.001 | 0.27 (−0.03, 0.53) | 0.075 | 0.04b (−0.28, 0.35) | 0.823 | |
| Organization | 0.50 (0.23, 0.70) | 0.0004 | 0.36 (0.06, 0.59) | 0.018 | 0.04b (−0.28, 0.35) | 0.787 | |
| Divided attention | 0.52 (0.25, 0.71) | 0.0003 | 0.24 (−0.06, 0.51) | 0.115 | −0.09b (−0.39, 0.23) | 0.582 | |
| Caregiver ECog | Memory | 0.60 (0.37, 0.76) | <0.0001 | 0.31 (0.01, 0.56) | 0.040 | −0.24b (−0.52, 0.08) | 0.135 |
| Language | 0.48 (0.21, 0.68) | 0.001 | 0.15 (−0.15, 0.43) | 0.319 | −0.28b (−0.55, 0.03) | 0.075 | |
| Visuospatial abilities | 0.16c (−0.17, 0.46) | 0.329 | 0.14c (−0.19, 0.44) | 0.413 | −0.09d (−0.41, 0.24) | 0.595 | |
| Planning | 0.41e (0.12, 0.64) | 0.007 | 0.34e (0.03, 0.58) | 0.030 | −0.16f (−0.46, 0.17) | 0.335 | |
| Organization | 0.41f (0.10, 0.65) | 0.009 | 0.22f (−0.12, 0.50) | 0.196 | −0.20g (−0.50, 0.14) | 0.240 | |
| Divided attention | 0.58e (0.34, 0.75) | <0.0001 | 0.37e (0.07, 0.61) | 0.016 | −0.19f (−0.49, 0.14) | 0.252 | |
Correlations between the domains of subjective cognition and symptom distress, household tasks performance, and workplace productivity stratified by post-transplant employment status.
Note: Bold values denote statistical significance at the p < 0.05 level.
n = 15.
n = 39.
n = 38.
n = 36.
n = 41.
n = 37.
n = 35.
Associations Between Objective Cognition and Patient-Reported Outcomes
Objective test scores of LT recipients were not associated with any patient-reported outcomes within the entire sample (Table 3). In employed recipients, higher global cognition (RBANS total score) was related to lower RSCL-M scores (β = −0.02, p = 0.018; Table 5).
Discussion
This cross-sectional study, to our knowledge, is the first to examine relationships between subjective and objective cognition and patient-reported outcomes of physical and psychological symptom distress, ability to perform household tasks, and workplace productivity among LT recipients. We found higher LT recipient self-rated cognitive decline was associated with higher physical symptom distress and workplace productivity loss. Higher caregiver-rated cognitive decline was associated with lower household tasks performance. However, these associations appear to be related to post-transplant employment status of LT recipients (employed vs. not employed). Cognitive decline measured by objective cognitive tests was not significantly associated with any of the patient-reported outcomes. These findings may suggest that LT recipients’ quality of life can be assessed with markers of subjective cognition, regardless of objective cognition.
Cognitive decline is one of the major health issues among LT recipients. Cognition, however, is not regularly assessed in transplant practice due to multiple reasons, including lengthy cognitive tests. Subjective cognition that is easily assessed by a valid and reliable self-report survey has potential to be used as a proxy for objective cognition at a busy transplant clinic. Most participants completed the ECog within 2 min (15). While we have shown that there are fair to moderate correlations between objective and subjective cognition among LT recipients (15), the present study highlights that these different cognitive measures may provide complementary information, particularly regarding patient-reported outcomes that require cognitive skills, such as workplace productivity.
Subjective cognition, not objective cognition, was associated with LT recipients’ perceived health-related quality of life and independence. While objective cognitive decline may contribute to develop worse clinical outcomes, such as graft failure and mortality (37), subjective cognitive decline may affect LT recipients’ overall quality of life (38). Recipient self-rated cognition, however, was not associated with psychological symptom distress. This finding was inconsistent with the literature in general (39) and chronic illness populations (40) that documented strong relationships between subjective cognitive decline and psychological symptoms. This unexpected finding may be related to the types of psychological symptoms assessed in this study. This study assessed overall mood state by measuring six different dimensions of mood (depression, vigor, confusion, tension, anger, and fatigue), while many previous studies were limited to the symptoms of depression and/or anxiety (39, 40). Additionally, this study recruited LT recipients regardless of their subjective cognitive status as opposed to intentionally recruiting individuals with cognitive complaints (39). Replication with a larger sample size that intentionally recruit LT recipients with cognitive complaints may advance the understanding of the associations between subjective cognition and psychological symptom distress in different dimensions of mood.
LT recipient self-rated cognition, not caregiver-rated cognition, was significantly correlated with physical symptom distress, indicating that LT recipients who experience subjective cognitive decline may also be experiencing higher levels of physical symptom distress. While the relationship between subjective cognition and physical symptoms, such as fatigue, has been documented in the chronic illness literature (41), the mechanism underlying this relationship has not been thoroughly examined. One possibility is that LT recipients who have subjective cognitive decline in memory and executive function, essential cognitive domains to self-manage, may believe that they are not capable to properly manage their physical symptoms. Their belief may reduce engagement in symptom monitoring and management, resulting in increased symptom distress.
Findings from this study may contribute to understanding the low employment rates among LT recipients. Consistent to previous studies in chronic disease populations (42), this study found a strong relationship between LT recipients’ subjective cognitive decline and self-reported workplace productivity loss. Particularly, LT recipients’ subjective ratings on memory and executive function, the core cognitive skills that are essential to perform job tasks, were correlated with the workplace productivity loss. Although these findings should be understood with caution due to a small sample size of employed LT recipients, they may suggest that subjective cognitive decline could be one of the barriers that prevent LT recipients from returning to work. Participating in work after LT is crucial to maintain independent and productive lives and reduce burden on recipients’ families and communities. Nevertheless, fewer than 25% of LT recipients are employed in paid work within 2 years post-transplant (43, 44). Findings of this study suggest an in-depth examination of the impacts of subjective and objective cognition on employment rates and workplace productivity to tackle unemployment among LT recipients.
Finally, this study provides insight into to the planning of individualized treatment to advance patient’s quality of life. Caregivers seem to be more accurate than patients themselves in estimating cognitive changes (15, 45). Their subjective ratings of LT recipients’ cognition may provide essential information regarding functional independence of LT recipients that can be used in the development of an individualized rehabilitation therapy. Further, employment status seems alter the associations between subjective cognition and patient-reported outcomes. While employed LT recipients have better subjective and objective cognition than non-employed recipients, their subjective cognition is more broadly associated with patient-reported outcomes than non-employed recipients’ subjective cognition. Such findings may imply that psychosocial circumstances of recipients, such as employment status, should be considered when planning a treatment for LT recipients.
A novel finding of this study is that subjective cognitive decline, not objective cognitive decline, is associated with LT recipients’ overall wellbeing. This study also suggests subjective cognition could be associated with low employment rate in this population. However, a few limitations of this study should be noted. Because of the cross-sectional nature of this study, the observed associations do not indicate cause and effect. The small sample recruited at a single center limits the generalizability of the study findings. Particularly, findings related to post-transplant employment status should be understood with caution due to the small sample size of employed LT recipients. Potential confounders that may affect the patient-reported outcomes, such as comorbidities and employment status before LT, were not included in the analysis.
In conclusion, LT recipients with subjective cognitive decline may benefit from extra support on improving their quality of life. In practice, clinicians may consider paying attention to LT recipients’ complaints about their cognition as they may reflect LT recipients’ poor quality of life. Clinicians may also consider including caregivers when developing an individualized post-LT care plan as these caregivers may provide supplemental information regarding LT recipients’ cognition and functional independence. Future longitudinal studies with a larger diverse sample are suggested to investigate the underlying mechanism of the relationships between subjective cognition and patient-reported outcomes. Such findings may contribute to identify strategies to support recipients with subjective cognitive decline to optimize their health and retain independence after LT.
Statements
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Vanderbilt University Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors contributed to the study design and acquisition of subjects and data. DK and KG were involved in the analysis and interpretation of the data and preparation of the manuscript. All authors read and approved the final manuscript.
Funding
This project was supported by CTSA awards Nos UL1 TR002243 and UL1TR002544 from the National Center for Advancing Translational Sciences. KG was supported by K23 AG045966 and R01 AG062826 from National Institute of Aging.
Acknowledgments
The authors thank Tara Fleckner for her statistical support. Study data were collected and managed using REDCap electronic data capture tools hosted at Vanderbilt University (17, 18).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Author disclaimer
This project’s contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Abbreviations
CI, confidence intervals; CTC, creative therapy consultants; ECog, everyday cognition; LT, liver transplant; MELD-Na, model for end-stage liver disease with sodium; NAB, neuropsychological assessment battery; POMS-SF, profile of mood states-short form; RBANS, repeatable battery for the assessment of neuropsychological status; REDCap, research electronic data capture; RSCL-M, rotterdam symptom checklist-modified; SD, standard deviation; WLQ, work limitations questionnaire.
References
1.
KwongAJKimWRLakeJRSmithJMSchladtDPSkeansMAet alOPTN/SRTR 2019 Annual Data Report: Liver. Am J Transpl (2021) 21(S2):208–315. 10.1111/ajt.16494
2.
SerperMAsraniSVanWagnerLReesePPKimMWolfMS. Redefining Success after Liver Transplantation: From Mortality toward Function and Fulfillment. Liver Transpl (2022) 28(2):304–13. 10.1002/lt.26325
3.
BurraPGermaniGGnoatoFLazzaroSRussoFPCilloUet alAdherence in Liver Transplant Recipients. Liver Transpl (2011) 17:760–70. 10.1002/lt.22294
4.
MulderMBBorgsteedeSDDarwish MuradSLandmanCSMetselaarHJHunfeldNGM. Medication-Related Problems in Liver Transplant Recipients in the Outpatient Setting: A Dutch Cohort Study. Front Pharmacol (2021) 12:637090. 10.3389/fphar.2021.637090
5.
LevenEAAnnunziatoRHelcerJLieberSRKnightCSWlodarkiewiczCet alMedication Adherence and Rejection Rates in Older vs Younger Adult Liver Transplant Recipients. Clin Transpl (2017) 31:e12981. 10.1111/ctr.12981
6.
HudaANewcomerRHarringtonCKeeffeEBEsquivelCO. Employment after Liver Transplantation: A Review. Transpl Proc (2015) 47(2):233–9. 10.1016/j.transproceed.2014.10.022
7.
KoDBratzkeLC. Cognitive Function in Liver Transplant Recipients Who Survived More Than 6 Months. Prog Transpl (2020) 30(4):335–41. 10.1177/1526924820958144
8.
AhluwaliaVWadeJBWhiteMBGillesHSHeumanDMFuchsMet alLiver Transplantation Significantly Improves Global Functioning and Cerebral Processing. Liver Transpl (2016) 22(10):1379–90. 10.1002/lt.24498
9.
CampagnaFMontagneseSSchiffSBiancardiAMapelliDAngeliPet alCognitive Impairment and Electroencephalographic Alterations before and after Liver Transplantation: What Is Reversible?Liver Transpl (2014) 20(8):977–86. 10.1002/lt.23909
10.
DolanskyMAHawkinsMAWSchaeferJTSattarAGunstadJRedleJDet alAssociation between Poorer Cognitive Function and Reduced Objectively Monitored Medication Adherence in Patients with Heart Failure. Circ Heart Fail (2016) 9(12):e002475. 10.1161/CIRCHEARTFAILURE.116.002475
11.
KaiserJDietrichJAmiriMRüschelIAkbabaHHantkeNet alCognitive Performance and Psychological Distress in Breast Cancer Patients at Disease Onset. Front Psychol (2019) 10:2584. 10.3389/fpsyg.2019.02584
12.
JungMSZhangMAskrenMKBermanMGPeltierSHayesDFet alCognitive Dysfunction and Symptom burden in Women Treated for Breast Cancer: a Prospective Behavioral and fMRI Analysis. Brain Imaging Behav (2017) 11(1):86–97. 10.1007/s11682-016-9507-8
13.
GlanzBIDéganoIRRintellDJChitnisTWeinerHLHealyBC. Work Productivity in Relapsing Multiple Sclerosis: Associations with Disability, Depression, Fatigue, Anxiety, Cognition, and Health-Related Quality of Life. Value Health (2012) 15(8):1029–35. 10.1016/j.jval.2012.07.010
14.
Von AhDStoreySCrouchA. Relationship between Self-Reported Cognitive Function and Work-Related Outcomes in Breast Cancer Survivors. J Cancer Surviv (2018) 12(2):246–55. 10.1007/s11764-017-0664-6
15.
KoDDietrichMSGiffordKARidnerSH. Subjective Cognition Reported by Caregivers Is Correlated With Objective Cognition in Liver Transplant Recipients. Liver Transpl (2022) 28(2):269–79. 10.1002/lt.26213
16.
VanceDEBailJEnahCPalmerJHoenigA. The Impact of Employment on Cognition and Cognitive reserve: Implications across Diseases and Aging. Nurs Res Rev (2016) 6:61–71. 10.2147/NRR.S115625
17.
HarrisPATaylorRThielkeRPayneJGonzalezNCondeJG. Research Electronic Data Capture (REDCap)—A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J Biomed Inform (2009) 42(2):377–81. 10.1016/j.jbi.2008.08.010
18.
HarrisPATaylorRMinorBLElliottVFernandezMO’NealLet alThe REDCap Consortium: Building an International Community of Software Platform Partners. J Biomed Inform (2019) 95:103208. 10.1016/j.jbi.2019.103208
19.
FariasSTMungasDReedBRCahn-WeinerDJagustWBaynesKet alThe Measurement of Everyday Cognition (ECog): Scale Development and Psychometric Properties. Neuropsychology (2008) 22(4):531–44. 10.1037/0894-4105.22.4.531
20.
FariasSTHussOChanMLRuizR. Revisions and Updates to the Everyday Cognition (ECog) Scales. Alzheimers Dement (2020) 16(6):e043263. 10.1002/alz.043263
21.
RandolphCTierneyMCMohrEChaseTN. The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS): Preliminary Clinical Validity. J Clin Exp Neuropsychol (1998) 20(3):310–9. 10.1076/jcen.20.3.310.823
22.
DuffKHobsonVLBeglingerLJO’BryantSE. Diagnostic Accuracy of the RBANS in Mild Cognitive Impairment: Limitations on Assessing Milder Impairments. Arch Clin Neuropsychol (2010) 25(5):429–41. 10.1093/arclin/acq045
23.
AcetoPPerilliVLaiCCiocchettiPVitaleFSollazziL. Postoperative Cognitive Dysfunction after Liver Transplantation. Gen Hosp Psychiatry (2015) 37(2):109–15. 10.1016/j.genhosppsych.2014.12.001
24.
Sánchez-CubilloIPeriáñEzJAAdrover-RoigDRodríGuez-SáNchezJMRíOs-LagoMTirapuJet alConstruct Validity of the Trail Making Test: Role of Task-Switching, Working Memory, Inhibition/interference Control, and Visuomotor Abilities. J Int Neuropsychol Soc (2009) 15:438–50. 10.1017/S1355617709090626
25.
WatersGSCaplanD. The Reliability and Stability of Verbal Working Memory Measures. Behav Res (2003) 35(4):550–64. 10.3758/BF03195534
26.
McKinlayA. Rey Complex Figure Test. In: Encyclopedia of Child Behavior and Development. Boston, MA: Springer (2011). p. 1264–5. 10.1007/978-0-387-79061-9_2437
27.
StraussEShermanEMSSpreenO. A Compendium of Neuropsychological Tests. third. New York: Oxford University Press (2006). p. 811.
28.
BerryDTRAllenRSSchmittFA. Rey-Osterrieth Complex Figure: Psychometric Characteristics in a Geriatric Sample. Clin Neuropsychol (1991) 5(2):143–53. 10.1080/13854049108403298
29.
SteinKDDennistonMBakerFDentMHannDMBushhouseSet alValidation of a Modified Rotterdam Symptom Checklist for Use with Cancer Patients in the United States. Pain Symptom Manage (2003) 26(5):975–89. 10.1016/S0885-3924(03)00321-X
30.
CurranSLAndrykowskiMAStudtsJL. Short Form of the Profile of Mood States (POMS-SF): Psychometric Information. Psychol Assess (1995) 7(1):80–3. 10.1037/1040-3590.7.1.80
31.
Creative Therapy Consultants. Evaluating a Homemaking Assessment for Broader Application to Practice (2016). www.creativetherapyconsultants.ca/publications/# (Accessed April 28, 2018).
32.
Creative Therapy Consultants. The Creative Therapy Consultants Homemaking Assessment: Administration Guide (2016). www.creativetherapyconsultants.ca/publications/# (Accessed April 28, 2018).
33.
LernerDAmick BC 3rdLeeJCRooneyTRogersWHChangHet alRelationship of Employee-Reported Work Limitations to Work Productivity. Med Care (2003) 41(5):649–59. 10.1097/01.MLR.0000062551.76504.A9
34.
LernerDAmickBCRogersWHMalspeisSBungayKCynnD. The Work Limitations Questionnaire. Med Care (2001) 39(1):72–85. 10.1097/00005650-200101000-00009
35.
Mapi Research Trust. Work Limitations Questionnaire Version 1.0: Scaling and Scoring. Lyon, France: Mapi Research Trust (2018).
36.
KimWRBigginsSWKremersWKWiesnerRHKamathPSBensonJTet alHyponatremia and Mortality Among Patients on the Liver-Transplant Waiting List. N Engl J Med (2008) 359(10):1018–26. 10.1056/NEJMoa0801209
37.
ThomasAGRuckJMShafferAAHaugenCEYingHWarsameFet alKidney Transplant Outcomes in Recipients with Cognitive Impairment: A National Registry and Prospective Cohort Study. Transplantation (2019) 103(7):1504–13. 10.1097/TP.0000000000002431
38.
LyckeMLefebvreTPottelLPottelHKetelaarsLStellamansKet alSubjective, but Not Objective, Cognitive Complaints Impact Long-Term Quality of Life in Cancer Patients. J Psychoso Oncol (2019) 37(4):427–40. 10.1080/07347332.2018.1504154
39.
ZlatarZZMunizMGalaskoDSalmonDP. Subjective Cognitive Decline Correlates with Depression Symptoms and Not with Concurrent Objective Cognition in a Clinic-Based Sample of Older Adults. J Gerontol B Psychol Sci Soc Sci (2018) 73(7):1198–202. 10.1093/geronb/gbw207
40.
D’hoogheMBDe CockAVan RemoortelABenedictRHBEelenPPeetersEet alCorrelations of Health Status Indicators with Perceived Neuropsychological Impairment and Cognitive Processing Speed in Multiple Sclerosis. Mult Scler Relat Disord (2019) 39:101904. 10.1016/j.msard.2019.101904
41.
NicolCOwnsworthTCubisLNguyenWFooteMPinkhamMB. Subjective Cognitive Functioning and Associations with Psychological Distress in Adult Brain Tumour Survivors. J Cancer Surviv (2019) 13(5):653–62. 10.1007/s11764-019-00784-8
42.
ChokkaPBougieJRampakakisEProulxJ. Assessment in Work Productivity and the Relationship with Cognitive Symptoms (AtWoRC): Primary Analysis from a Canadian Open-Label Study of Vortioxetine in Patients with Major Depressive Disorder (MDD). CNS Spectr (2019) 24(3):338–47. 10.1017/S1092852918000913
43.
HudaANewcomerRHarringtonCBlegenMGKeeffeEB. High Rate of Unemployment after Liver Transplantation: Analysis of the United Network for Organ Sharing Database. Liver Transpl (2012) 18:89–99. 10.1002/lt.22408
44.
SaabSWieseCIbrahimABPeraltaLDurazoFHanSet alEmployment and Quality of Life in Liver Transplant Recipients. Liver Transpl (2007) 13(9):1330–8. 10.1002/lt.21247
45.
MillerLSBrownCLMitchellMBWilliamsonGM. Activities of Daily Living Are Associated with Older Adult Cognitive Status: Caregiver versus Self-Reports. J Appl Gerontol (2013) 32(1):3–30. 10.1177/0733464811405495
Summary
Keywords
cognitive function, subjective cognition, patient-reported outcomes, symptom distress, work productivity, liver transplant recipients
Citation
Ko D, Ridner SH and Gifford KA (2023) Subjective Cognition is Related to Patient-Reported Symptom Distress and Work Productivity Among Liver Transplant Recipients. Transpl Int 36:10863. doi: 10.3389/ti.2023.10863
Received
25 August 2022
Accepted
02 January 2023
Published
17 January 2023
Volume
36 - 2023
Updates
Copyright
© 2023 Ko, Ridner and Gifford.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dami Ko, d.ko@northeastern.edu
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.