Abstract
Aim:
To present a rare and complex case of a spontaneous intercostal, transdiaphragmatic and abdominal wall hernia in an elderly male with a history of chronic obstructive pulmonary disease (COPD).
Methods:
According to the CARE checklist, we describe a rare case of intercostal, transdiaphragmatic and abdominal wall hernia after an episode of severe coughing.
Results:
A 72-year-old male presented with nausea, dyspnea, and progressive left thoracic and abdominal swelling, along with a history of severe cough and spontaneous hematoma in the same regions. A CT scan revealed an intercostal hernia between the 8th and 9th ribs, with transdiaphragmatic extension and involvement of the lateral abdominal wall, containing most of the stomach, transverse colon, splenic flexure, descending colon, and small intestine. An elective left thoraco-abdominal open surgery was performed, including preperitoneal hernioplasty with dual mesh placement and repair of the diaphragmatic and costal defect.
Conclusion:
Such cases are scarcely reported in the literature. This case highlights the importance of considering complex hernia in patients with severe COPD and the importance of early treatment along with a multidisciplinary surgical approach.
Introduction
Intercostal, transdiaphragmatic, and abdominal wall hernias are exceptionally rare due to the extensive nature of the hernia and the involvement of multiple compartments, including thoracic and abdominal cavities [1]. When the abdominal viscera gain entry to the intercostal space through an associated diaphragmatic defect, the term of transdiaphragmatic intercostal hernia is usually employed, where as if no diaphragmatic abnormality is present, the term abdominal intercostal hernia (AIH) is used [2, 3]. These types of hernia are almost always located inferiorly to the ninth rib and are predominantly found on the left thoracic side [3, 4]. They usually occur after trauma, but less frequently, increased intrathoracic pressure during episodes of severe coughing can cause a hernia, although this is rarely reported [2].
Case Description
We report the case of a 72-year-old male, former smoker, with a medical history of arterial hypertension, diabetes mellitus, and chronic obstructive pulmonary disease (COPD). He was hospitalized in December 2023 for community-acquired pneumonia.
In February and March 2024, the patient presented to the emergency department with symptoms including nausea, dyspnea, and progressively increasing left-sided thoracic and abdominal swelling. He reported experiencing a severe cough following the pneumonia episode, which was soon followed by the spontaneous appearance of a hematoma on the left hemithorax and hemiabdomen. On physical examination, significant left-sided thoracic and abdominal swelling was observed, along with clinical signs suggestive of a partially reducible hernia (Figure 1).
FIGURE 1
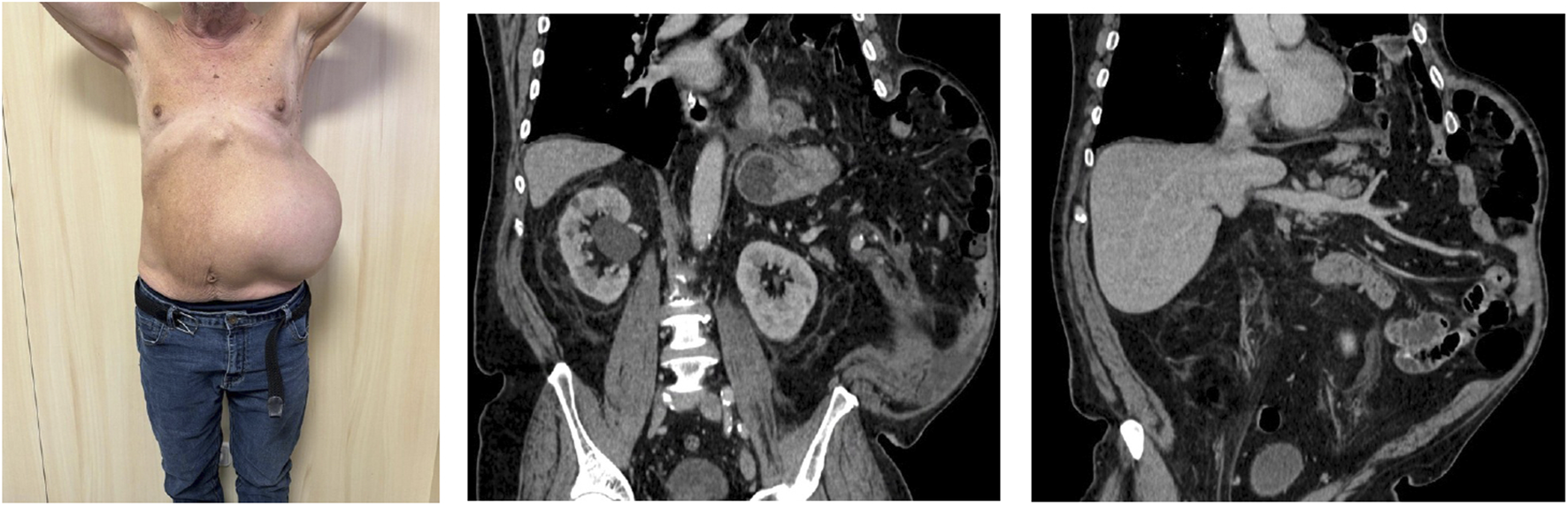
Patient and preoperative CT scan.
A computed tomography (CT) scan revealed an intercostal hernia between the eighth and ninth ribs, extending transdiaphragmatically and involving the left lateral abdominal wall. The hernia sac contained the majority of the stomach, colon and loops of small bowel (Figure 1). The patient underwent preoperative optimization, including prehabilitation focused on weight loss and control of COPD to minimize the risk of hernia exacerbation.
In April 2024, the patient underwent an elective open thoracoabdominal hernia repair. Intraoperative findings included a 9 × 9 cm defect in the internal oblique and transversus abdominis muscles, with costal cartilage disinsertion between the 8th and 9th ribs, as well as an 8 cm diaphragmatic defect. The hernia sac extended into the left abdominal wall, intrathoracic, and intercostal regions.
A preperitoneal hernioplasty was performed using Bio-A and polypropylene mesh to reinforce the abdominal wall (Figure 2). The diaphragmatic defect was repaired and reinforced with a Synecor mesh (Figure 3). Thoracic surgeons closed the intercostal space and placed a thoracic drain, ensuring closure of the communication between the preperitoneal lateral space and the thoracic cavity.
FIGURE 2
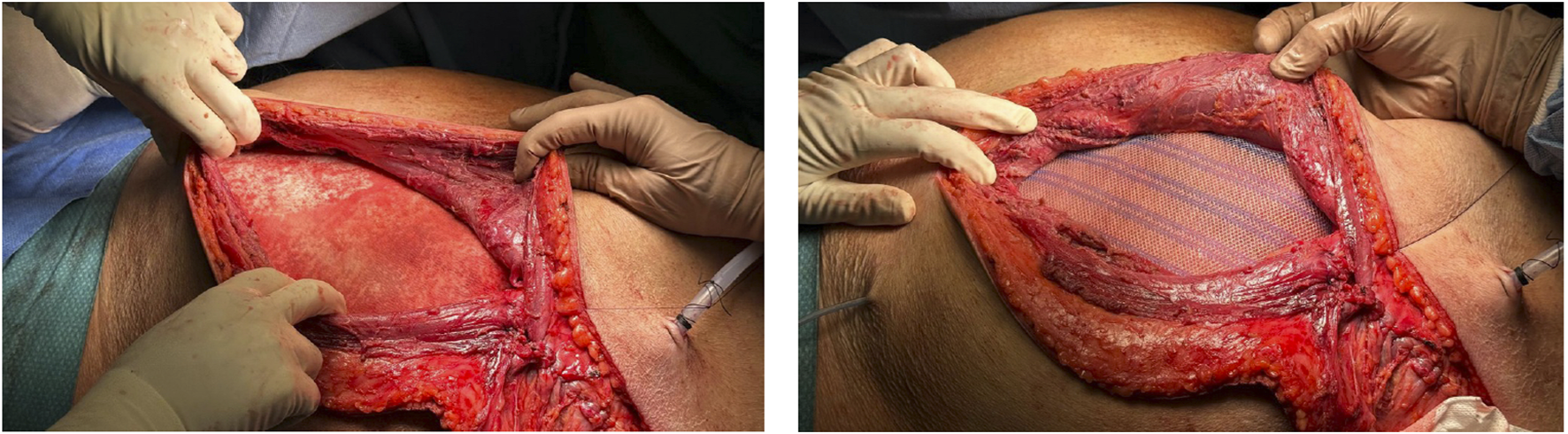
Preperitoneal hernioplasty (Bio-A and polypropylene mesh).
FIGURE 3
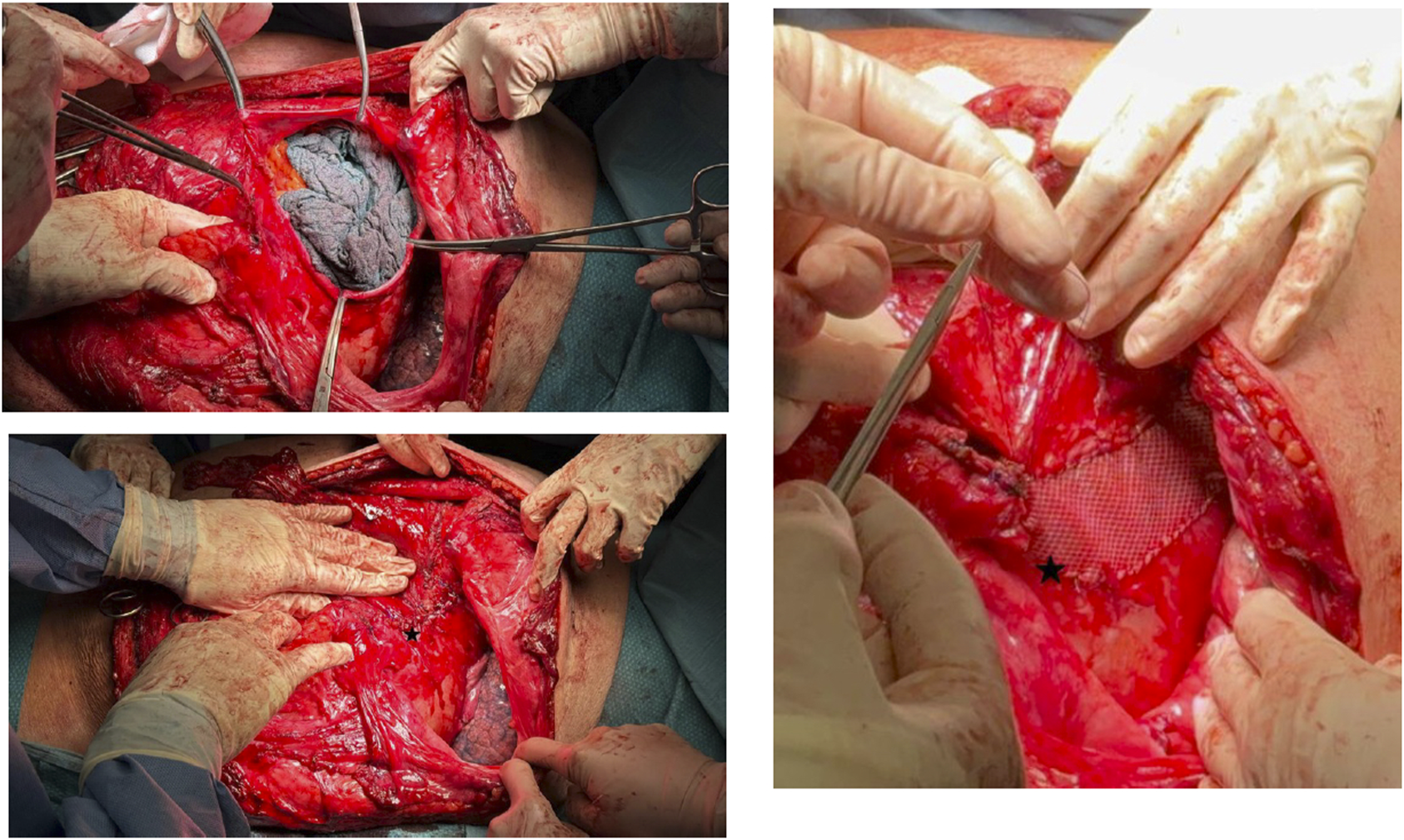
Closure of the diaphragmatic defect with reinforcement mesh.
During hospitalization, an episode of renal insufficiency exacerbation occurred, which was successfully managed with targeted therapy. He was discharged after 11 days with no further complications.
At 6-month follow-up, the only significant finding was a minor subcutaneous seroma at the site of the thoracic incision. There were no reports of abdominal or thoracic discomfort, dyspnea, or other complications. The patient continued respiratory rehabilitation, showing effective management of his COPD.
Discussion
This is a rare pathology in clinical practice, and much of the existing literature consists of case reports. Systematic reviews on this topic highlight the absence of a standardized classification system to guide the management of the various types of hernias, given the diversity in their presentations [5, 6]. These hernias are typically classified as either acquired or spontaneous [1–3, 7, 8]. Acquired hernias are generally secondary to major trauma, such as penetrating injuries, falls, or crush injuries [5], as well as to minor trauma, such as a sudden increase in thoracic pressure caused by severe coughing, childbirth, physical exertion, or vomiting [1–4, 7, 9, 10]. However, in spontaneous cases, the literature reveals that patients often report chronic coughing related to smoking, COPD, obesity, advanced age, or collagenopathies [1, 2, 7, 11, 12]. It remains debatable whether these cases are truly spontaneous or result from repeated minor trauma over time. In our view, this type of hernia should always be considered acquired, either through an acute traumatic event or through chronic, repeated minor trauma from increases in thoraco-abdominal pressure.
The lack of consistency in the literature complicates the identification and management of these cases. In 1978, Le Neel et al. described four cases of what they termed “abdominal intercostal hernia,” defining it as the protrusion of abdominal viscera through an intercostal space following diaphragmatic herniation and intercostal muscle rupture [11]. Since then, this term has been used globally, often without specifying the anatomical areas involved. Gooseman et al. introduced the Sheffield classification, which considers the involvement of costal margin rupture, diaphragmatic rupture, and intercostal rupture [6]. More recently, Byers et al. analyzed management strategies based on this classification, distinguishing between conservative and surgical approaches [5]. Patients with isolated costal margin rupture often benefit from conservative management, with favorable outcomes, while diaphragmatic and/or intercostal ruptures typically require surgical repair [5]. We propose that the involvement of abdominal wall musculature should be integrated into the classification system, as this component is frequently overlooked but crucial in cases like the one presented. Proper management in such cases extends to abdominal wall repair.
A comprehensive, standardized classification system is critical to optimize the management of this pathology and achieve better clinical outcomes. Conventional CT and 3D imaging are generally employed to detect all anatomical defects [5]. While chest X-rays and ultrasound may also be used, they are less effective [13].
The surgical approach is not yet standardized, but it is essential to repair all components of the defect, including the diaphragm, intercostal muscles, abdominal wall, and costal margin, to minimize recurrence and postoperative pain. Open surgery via thoracic or thoracoabdominal incision remains the most common approach [5]. However, there are reports of successful laparoscopic repair, offering early mobilization and minimal postoperative discomfort, though with limited long-term follow-up [4, 14]. Early surgical intervention in scheduled cases can prevent complications such as incarceration, which significantly increases morbidity and mortality [10, 15, 16].
In conclusion, early surgical intervention is key to preventing complications. This case illustrates a rare and complex hernia that can develop in patients with severe COPD, especially after intense coughing. In this case, the severe post-pneumonia cough likely caused the rupture of the diaphragm and abdominal wall, leading to herniation. The strengths of this case include a successful multidisciplinary surgical approach and a favorable postoperative outcome. However, the patient’s underlying pulmonary condition presents a risk of hernia recurrence. This case adds to the limited body of literature on such hernias, underscoring the importance of meticulous preoperative planning and postoperative management in similar cases.
Statements
Data availability statement
The datasets presented in this article are not readily available because data about the patient is confidential. Requests to access the datasets should be directed to the local informatic health care system.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
Literature review and drafting of the manuscript: PM-L and ML-C. Critical revision: MV-T, VR-G, and AM-D-R. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
ML-C is currently the Editor-in-Chief of JAWS and he has received honoraria for consultancy, lectures, support for travels and participation in review activities from BD, Medtronic and Gore.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Abu-Gazala M Ratnayake A Abu-Gazala S Bala M . An Enigma of Spontaneous Combined Transdiaphragmatic, Intercostal and Abdominal Wall Hernia. Hernia : J hernias Abdom wall Surg (2013) 17(3):415–8. 10.1007/s10029-012-0902-9
2.
Unlu E Temizoz O Cagli B . Acquired Spontaneous Intercostal Abdominal Hernia: Case Report and a Comprehensive Review of the World Literature. Australas Radiol (2007) 51(2):163–7. 10.1111/j.1440-1673.2006.01661.x
3.
Erdas E Licheri S Calò PG Pomata M . Acquired Abdominal Intercostal Hernia: Case Report and Systematic Review of the Literature. Hernia : J hernias Abdom wall Surg (2014) 18(5):607–15. 10.1007/s10029-014-1232-x
4.
Bobbio A Ampollini L Prinzi G Sarli L . Endoscopic Repair of an Abdominal Intercostal Hernia. Surg Laparosc Endosc and percutaneous Tech (2008) 18(5):523–5. 10.1097/SLE.0b013e31817f2883
5.
Byers JL Rao JN Socci L Hopkinson DN Tenconi S Edwards JG . Costal Margin Injuries and Trans-diaphragmatic Intercostal Hernia: Presentation, Management and Outcomes According to the Sheffield Classification. The J Trauma acute Care Surg (2023) 95(6):839–45. 10.1097/TA.0000000000004068
6.
Gooseman MR Rawashdeh M Mattam K Rao JN Vaughan PR Edwards JG . Unifying Classification for Transdiaphragmatic Intercostal Hernia and Other Costal Margin Injuries. Eur J cardio-thoracic Surg : official J Eur Assoc Cardio-thoracic Surg (2019) 56(1):150–8. 10.1093/ejcts/ezz020
7.
Gupta V Singhal R Ansari MZ . Spontaneous Rupture of the Diaphragm. Eur J Emerg Med : official J Eur Soc Emerg Med (2005) 12(1):43–4. 10.1097/00063110-200502000-00013
8.
Ampollini L Cattelani L Carbognani P Rusca M . Spontaneous Abdominal--Intercostal Hernia. Eur J cardio-thoracic Surg : official J Eur Assoc Cardio-thoracic Surg (2011) 39(2):275. 10.1016/j.ejcts.2010.05.040
9.
Khan AS Bakhshi GD Khan AA Kerkar PB Chavan PR Sarangi S . Transdiaphragmatic Intercostal Hernia Due to Chronic Cough. Indian J Gastroenterol : official J Indian Soc Gastroenterol (2006) 25(2):92–3.
10.
Lund EP Bergenfeldt M Burcharth F . Traumatic Abdominal Hernia Caused by Cough, Presenting with Intestinal Obstruction. Hernia : J hernias Abdom wall Surg (2004) 8(4):399–401. 10.1007/s10029-004-0249-y
11.
Le Neel JC Mousseau PA Leborgne J Horeau JM Labour PE Mousseau M . La hernie intercostale abdominale. Rapport de quatre observations [Abdominal intercostal hernia. Report of four cases (author's transl)]. Ann de chirurgie (1978) 32(2):138–41.
12.
Chapman AA Duff SB . A Case of Spontaneous Transdiaphragmatic Intercostal Hernia with Contralateral Injury, and Review of the Literature. Case Rep Surg (2017) 2017:7416092. 10.1155/2017/7416092
13.
Sharma OP Duffy B . Transdiaphragmatic Intercostal Hernia: Review of the World Literature and Presentation of a Case. The J Trauma (2001) 50(6):1140–3. 10.1097/00005373-200106000-00026
14.
Kurer MA Bradford IM . Laparoscopic Repair of Abdominal Intercostal Hernia: A Case Report and Review of the Literature. Surg Laparosc Endosc and percutaneous Tech (2006) 16(4):270–1. 10.1097/00129689-200608000-00017
15.
Lasithiotakis K Venianaki M Tsavalas N Zacharioudakis G Petrakis I Daskalogiannaki M et al Incarcerated Spontaneous Transdiaphragmatic Intercostal Hernia. Int J Surg case Rep (2011) 2(7):212–4. 10.1016/j.ijscr.2011.07.002
16.
Bennet S Wang M Spiro C Tog C . Gastric Volvulus and Tension Gastrothorax Secondary to Spontaneous Transdiaphragmatic Intercostal Hernia. BMJ case Rep (2022) 15(1):e246832. 10.1136/bcr-2021-246832
Summary
Keywords
intercostal hernia, transdiaphragmatic hernia, abdominal wall hernia, chronic obstructive pulmonary disease, cough
Citation
Martínez-López P, Verdaguer-Tremolosa M, Rodrigues-Gonçalves V, Martín-Del-Rey A and López-Cano M (2025) Case Report: Combined Intercostal-Transdiaphragmatic-Abdominal Wall Hernia. J. Abdom. Wall Surg. 4:14535. doi: 10.3389/jaws.2025.14535
Received
24 February 2025
Accepted
23 June 2025
Published
04 July 2025
Volume
4 - 2025
Updates
Copyright
© 2025 Martínez-López, Verdaguer-Tremolosa, Rodrigues-Gonçalves, Martín-Del-Rey and López-Cano.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: P. Martínez-López, pilarmartinezlopez3@gmail.com; M. López-Cano, mlpezcano@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.