Abstract
Background: Laparoscopic and robot-assisted surgery is now common place, and each trocar site is a potential incisional hernia site. A number of factors increase the risk of trocar site hernia (TSH) at any given trocar site. The aim of this paper is to explore the literature and identify the patients and the trocar sites at risk, which may allow target prevention strategies to minimise TSH.
Methods: A pub med literature review was undertaken using the MeSH terms of “trocar” OR “port-site” AND “hernia.” No qualifying criteria were applied to this initial search. All abstracts were reviewed by the two authors to identify papers for full text review to inform this narrative review.
Results: 961 abstracts were identified by the search. A reasonable quality systematic review was published in 2012, and 44 additional more recent publications were identified as informative. A number of patient factors, pre-operative, intra-operative and post-operative factors were identified as possibly or likely increasing the risk of TSH. Their careful management alone and more likely in combination may help reduce the incidence of TSH.
Conclusion: Clinically symptomatic TSH is uncommon, in relation to the many trocars inserted every day for “keyhole” surgery, although it is a not uncommon hernia to repair in general surgical practice. There are patients inherently at risk of TSH, especially at the umbilical location. It is likely, that a multi-factored approach to surgery, will have a cumulative effect at reducing the overall risk of TSH at any trocar site, including choice of trocar type and size, method of insertion, events during the operation, and decisions around the need for fascial closure and how this is performed following trocar removal.
Introduction
Laparoscopic and more recently robot-assisted laparoscopic surgery for both benign and malignant conditions of the abdomen has become common place. This was seen from the early 1990’s with the rapid change in practice from open to laparoscopic cholecystectomy (1). Much of the early surgery involved a camera port placed at the umbilicus, and a variety of other ports inserted to allow not only diagnostic but therapeutic interventions. As opposed to one incision, much of laparoscopy involves several small incisions, with each trocar site a possible incisional hernia site. Incisional hernia at a trocar site is often referred to as a “trocar site hernia” (TSH), and it is perhaps better referred to as this rather than a “port site hernia,” as PSH can be confused with the abbreviation for parastomal hernia.
The prevalence of TSH is unclear (2, 3). Imaging such as ultrasound and CT scans appear to diagnose many more TSH than are clinically detectable, and also help clarify the diagnosis when a TSH is clinically suspected (4-7). For example, the TSH incidence in laparoscopic bariatric surgery is usually said to be low single figures of a percent (4). However, in a prospective cohort series with ultrasound follow in a similar study population, one or more of the trocar sites had developed a TSH in 34% of patients (8). This finding has to be set against a follow up CT scan study in a similar study population (the CT scan was done for other reasons but was reviewed for the study). The study included 244 patients, with 732 port sites of 11 or 12 mm diameter, but only 2 fascial defects were identified—all non-palpable, asymptomatic and plugged with fat (9). Clinical versus imaging diagnosis, and the protocol for the imaging, such as with or without Valsalva, may influence detection of TSH. While many small TSHs may have a long natural history of developing into a clinically overt hernia, the explosion in laparoscopic surgery over the last 30 years has not resulted in a similar explosion in the number of TSHs presenting to the surgeon for repair. Indeed, TSH is still a relatively uncommon hernia requiring surgical repair.
Nevertheless, TSHs are evident, and many that present with symptoms of a bulge and/or pain, do require repair, including a small number that present acutely, sometimes within days of the original surgery. Thus, prevention of TSH is likely to be of benefit to patients undergoing laparoscopic surgery. The aim of this narrative review, was to provide an overview of steps along the patient journey that might reduce the risk of TSH. These include possible pre-operative factors, patient risk factors, intra-operative factors as well as post-operative events.
Methods
A pub med literature review was undertaken on 29 August 2022. The MeSH terms of “trocar” OR “port-site” AND “hernia” was undertaken. There was no attempt at limitation of the search. Papers of any study type including case reports, human and animal research, any language were allowable in the initial search. The title and abstract of the papers from the literature search were scanned by both authors, and possible papers for inclusion selected. Where there was disagreement this was discussed, and generally the abstract included for full text review. Further full text articles were excluded if duplicate information or were not relevant to this review. The focus of this paper was pure TSH, and incisional hernias related to specimen extraction sites, where the trocar site was enlarged, were not included in this review. It was hoped that a reasonable quality systematic or narrative review on TSH in the last 10 years would be identified, and thus limit this review to an update with more recent publications.
A number of topics were considered when reviewing the abstracts and full text papers. These topics were re-operative or patient factors, trocar location, technique of trocar insertion, trocar type, size, length of operation, closure of trocar site and post-operative rehabilitation.
Results and Discussion
The Prisma flow chart of the publications reviewed is shown in Figure 1. The quality of evidence was generally low, with over half (24 of the 45 publications included) retrospective cohort series. A systematic review published in 2012 was identified (2), and this was used to eliminate studies published prior to this date.
FIGURE 1
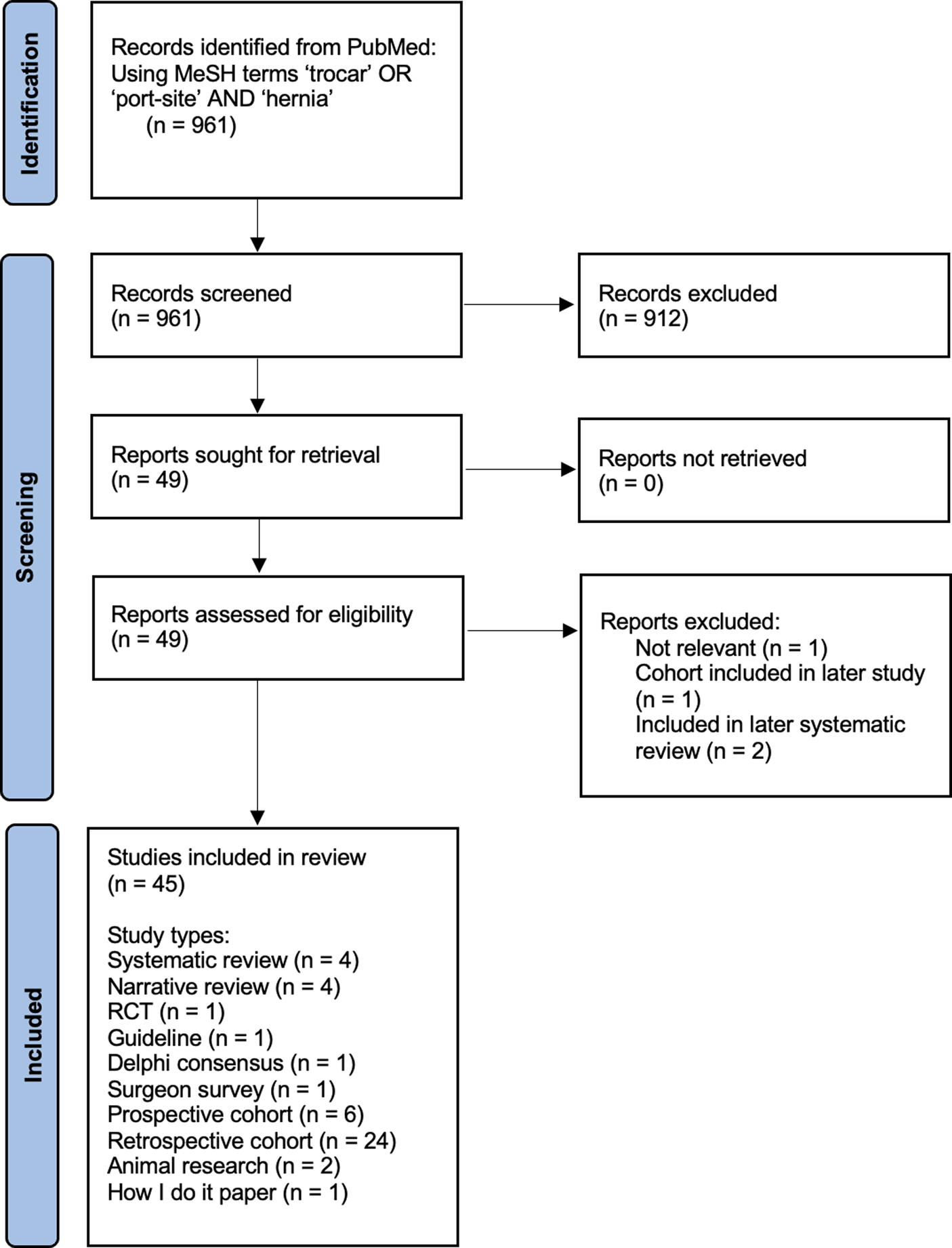
Prisma Flow chart of PubMed Search.
Pre-Operative or Patient Factors
TSHs are in essence a particular form of incisional hernia. It is not surprising that general risk factors for incisional hernia are also seen for TSH. Namely smoking, obesity, connective tissue disorders, systemic disease such as diabetes mellitus, immunosuppression, the elderly or frail, and sarcopenia, along with rectus diastasis and a history of a previous hernia elsewhere (10-13).
Of interest to this paper on TSH, is the conflicting evidence around pre-existing hernias at the site of the trocar or hernias elsewhere on the abdominal wall. The presence of an umbilical hernia is a risk factor for a TSH at the umbilicus (13, 14). But the water is muddied on this topic by nomenclature. Is the resultant hernia a TSH, a recurrent umbilical hernia or indeed more correctly termed an incisional hernia? And how the umbilical hernia was managed in terms of closure at the end of the operation may also influence the TSH rates. But in a study of umbilical TSH after laparoscopic TAPP inguinal hernia surgery, umbilical TSH was related to the pre-operative presence of an umbilical hernia, rectus abdominis diastasis and surgery for a recurrent inguinal hernia (13).
For many of these patients, pre-habilatation with weight loss, exercise, reducing immunosuppression drugs where possible and reducing the degree of sarcopenia will likely reduce the TSH rate, although evidence that such interventions reduce TSH is lacking in this area. Avoidance of the umbilicus when there is a concomitant umbilical hernia may reduce the TSH rate. Although the patient will still have their umbilical hernia—so it could be argued that in patients with an umbilical hernia, this is the preferred site so that umbilical hernia repair can be incorporated into the surgery.
Trocar Location Choices: Umbilicus, Midline, off Midline
The umbilicus has been for many laparoscopic operations, the first port insertion site, the usual camera location and often in addition, the specimen extraction location. Given the common co-existence of an umbilical hernia, it is not surprising that the umbilicus seems to be the most common site of TSH (14-16). In a cohort series of laparoscopic bariatric operations undergoing follow up CT scanning, performed prone, the umbilicus was by far the commonest site of TSH (17). However, at the time of writing the study (17), none of the patients identified with a TSH had undergone repair, with nearly all were asymptomatic. Yet in bariatric surgery, most surgeons now would try and avoid the umbilicus, not necessarily purely for TSH prevention, but the fact that the umbilical site is often too far away from the operative field in the left upper quadrant.
Similarly, epigastric trocars, used in the common operation of laparoscopic cholecystectomy, has a TSH incidence muddled by this trocar location often being enlarged for gallbladder extraction (12). But trocars inserted in the midline do seem to have a higher TSH rate, even when closure of the linea alba defect is attempted. The midline insertion is often quick, and the relatively avascular midline does have some advantages over the risk of bleeding when trocars are inserted through the belly of the rectus muscle for example, and especially in the lower half of the abdomen where the inferior epigastric vessels are at risk of injury. In the end of the day, port location is partly determined by the operation being undertaken, but TSH can be reduced if the midline is avoided (18).
Trocar Insertion Technique: Open v Closed
The open or cut down technique, especially for the first camera port has been promoted as a standard of care at the umbilicus. Again, prevention of a TSH is not the main factor here, rather safe entry to the abdominal cavity. However, open insertion techniques “under vision” are not so easy away from the umbilicus, especially in the obese. While an open cutdown will likely result in a larger “hole” in the abdominal wall, the ability to see the aponeurotic layers at the time of formation and place sutures accurately into these at the beginning of the operation may mitigate against this in terms of risk of TSH. The insertion of sutures at the end of the procedure, particularly when vision down a deep hole and identification especially of the posterior aponeurotic layer, may be less than ideal. A study comparing an open technique versus direct trocar insertion did report a lower incidence of TSH with the direct entry technique (19). Similarly, a study looking at lateral sited trocars reported similar findings (20).
Trocar Type Bladed/Cutting v Noncutting
Previous reviews have suggested that there is some evidence that cutting blades are associated with a higher TSH risk, compared to more “blunt” or tissues separating trocars (2, 16). Cutting trocars do in general pass more easily through the abdominal wall, but the use of less force during insertion may allow overshoot once the tip of the trocar is in the abdominal cavity. And a cutting tip is more likely to cut through a vessel in the abdominal wall on insertion, rather than push it aside as the trocar is inserted. The pressure effect of the trocar on the tissues may tamponade the vessel until the trocar is removed, and then bleeding commences. So there are reasons to avoid the use of cutting trocars, and they do seem to be less commonly available now.
A porcine animal model has demonstrated that a cutting trocar produces a similar size hole in the fascia compared to tissue separating trocars (21). While that may be true, the effect of cutting the tissues rather than spreading it on insertion, may be compounded over the course of the surgery as the instrument in the trocar is manipulated and forces applied to the abdominal wall.
Trocar Size: 12, 11, 10, 8, 5 mm
Port size, particularly in the midline does seem to influence TSH. However, TSH are reported even for the 8 mm robot-assisted trocars (22, 23), and indeed, more rarely, in 5 mm trocar sites (24).
Not surprisingly, large single port trocars, again often placed at the umbilicus, are associated with an increase in the TSH as reported in recent systematic reviews (25, 26). However, a number of cohort series have not demonstrated much if any difference in TSH between multi-port and single-port laparoscopic surgery (27).
Trocar Insertion: Vertical v Angled Towards Operative Field
In general, it is good surgical practice to insert a trocar vertically or perhaps more accurately, perpendicularly to the abdominal wall. Sometimes, a more angled approach, especially where surgery is undertaken in a limited area, such as a laparoscopic cholecystectomy or fundoplication, allows less torque feedback from the abdominal wall, making instrument manipulation through the trocar easier as there is less friction resistance to the instrument in the trocar. However, if the tip of the instrument works sometimes in the upper abdomen, and sometimes in the lower, then as the instrument and thus trocar is manipulated, there can be enlargement of the “hole” with tearing of the tissues of the abdominal wall. So careful insertion, under vision, taking stock of the likely location of surgery within the abdomen, and angling the trocar appropriately, may help reduce the secondary trauma the port may cause during the surgery. However, there is no evidence in the literature to support this common sense approach.
In robot-assisted surgery, an additional element is “port training.” This is a process at the start of surgery, and if the bed position is changed, where each arm of the robotic platform has to be educated about the pivot point or fulcrum—the part of the trocar held by the abdominal wall muscles—around which the robot arms perform their movement. If the pivot point, is not set correctly, then the trocar will pivot around a different set point, potentially causing shearing injury to the abdominal wall, enlarging the defect in the abdominal wall musculature/fascia.
The “Z approach” has been described to trocar insertion, with the location of the hole in the superficial fascia does not quite line up with the deep hole (28). However, no evidence around TSH prevention is presented in this paper to be able to make further comment on this.
Length of Operation
A number of studies have commented on an increasing TSH rate with increasing length of surgery (2, 24). Again, this is a difficult factor on its own to unravel. Longer operations are likely to be more difficult, involving more manipulation of the instruments and thus the trocars, and result in a more tired or distressed surgeon at the time of trocar site closure. Incorrect port training in robot assisted surgery may also compound this, the longer the operation continues. Which of these factors, if any, contribute to the higher TSH rate, is unknown.
Closure of the Trocar Site and What Technique?
It is generally accepted that closure of the umbilical trocar site, most midline trocar sites of 10 mm or more, and any port site that is enlarged for specimen extraction (this is a specific trocar site situation and is not discussed further) is good practice (18). An international consensus group had 86.8% agreement that closure of 15 mm ports in all patients was necessary (29). The closure of 10 mm and upwards (and also 8 mm in some robotic operations) trocar sites off the midline is less clear cut, with a broad spectrum of opinion from the “never close” to the “always close” surgeon (29, 30). A retrospective cohort series after laparoscopic sleeve gastrectomy, suggested that closure of the trocar site reduced the TSH incidence by two thirds (31). Another retrospective cohort group in a similar study population reported that closure of the 12 mm epigastric port halved the TSH incidence (32).
A number of closure techniques of trocar sites are described, including direct visualisation and simple suture as a single stitch or a figure of 8 stitch (33). Various needle types, and techniques to pass sutures either blindly or under some vision are reported with good results on short term follow up (34-40). Incorporating haemostats into the suture closure is also described (41, 42). A small series of 15 cases using a “mini-IPOM-plug” reported “good” 6 months outcomes (43). But none of these techniques, including some that have been in use for many years, have gained widespread adoption in surgical practice.
As mentioned above, the umbilicus is a relatively high risk site for TSH. Add in additional factors that makes the patient at higher risk for TSH in general, then perhaps mesh augmentation of the trocar site hernia would be a good idea. One of the few more recent randomised controlled trials, compared prophylactic mesh closure (intra-peritoneal polypropylene omega-3 mesh) versus suture at the umbilicus after laparoscopic cholecystectomy in patients identified as “high-risk” (44). 106 patients were randomised; 92 were included in the final analysis. The TSH rate was reduced in the mesh group to 4.4% compared to 31.9% in the suture group. The wound infection rate was lower in the mesh group (0% v 8.5%), but no other differences between the two groups were noted. The mesh used in this study has now been withdrawn from the market. In a non-randomised study of single port sleeve gastrectomy, both permanent and absorbable mesh reduced the TSH rate at 1 year (45). What mesh, which location of the abdominal wall, what mesh size, in which patient and so on remains unclear from the current literature.
Other techniques for trocar site closure are being considered. A recent study described “controlled heat-induced collagen denaturation” in a living pig model (46). Only 12 trocar sites in 3 pigs were reported on, so more work for sure is required before this potentially enters clinical practice.
Post-Operative Rehabilitation
There is no literature to help advise specifically on the prevention of TSH after surgery. Return to normal activities of daily living, work and sport is encouraged within the level of discomfort of the patient as is the advice following abdominal surgery in general. Activities that significantly increase intra-abdominal pressure, such as coughing, sneezing and jumping from a height, cannot be influenced to any great degree apart from the latter! Blaming the patient for doing too much too soon, is not an excuse for the resultant TSH.
Summary Discussion
Clinically symptomatic TSH is uncommon, in relation to the many trocars inserted every day for “keyhole’ surgery. The evidence around prevention of TSH is poor. Much of the literature is retrospective cohort studies and case reports with short term follow up from the original surgery. Prospective cohort series or interventional trials under the rigors of a RCT are few in number.
There will be patients inherently at risk of TSH, especially at the umbilical location, and to a lesser extent the whole of the midline. It is likely, that a multi-factored approach to surgery, will have a cumulative effect at reducing the overall risk of TSH at any trocar site, including choice of trocar type and size, method of insertion, events during the operation, and decisions around the need for fascial closure and how this is performed. Symptomatic TSH appears to be a lot lower than the true TSH rate, which is reassuring. Closure of a trocar site at the end of an operation appears to be surgeon individualised, from the “never closers,” to the “always closers” of 10 mm ports and above. Nevertheless, TSH repair remains a not uncommon elective and emergency hernia operation in view of the volumes of laparoscopic and robot-assisted surgery worldwide.
Future studies should focus on identifying the trocar sites at risk, which is likely to be a combination of patient factors, trocar site, trocar type and so on as mentioned above. This may help identify which trocar sites can be left unclosed, which trocar sites that merit suture closure, and which trocar sites that merit additional mesh augmentation. One of the more difficult areas to examine, which may well be an important element in the risk of TSH, is the surgeon as a risk factor. Knowledge about patients at risk, and training in the operative elements and decision making around trocar type, site, insertion technique and effective closure where necessary tailored to the patient, will likely help reduce the surgeon as an additional risk factor.
Statements
Author contributions
AB and BE were involved in design, literature search, and preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Talseth A Lydersen S Skjedlestad F Hveem K Edna T-H . Trends in Cholecystectomy Rates in a Defined Population during and after the Period of Transition from Open to Laparoscopic Surgery. Scand J Gastroenterol (2014) 49(1):92–8. 10.3109/00365521.2013.853828
2.
Swank HA Mulder IM la Chapelle CF Reitsma JB Lange JF Bemelman WA . Systematic Review of Trocar-Site Hernia. Br J Surg (2012) 99(3):315–23. 10.1002/bjs.7836
3.
De Alwis D Ades A Nanayakkara P . Laparoscopic Port-Site Hernia: An Underrecognized Iatrogenic Complication of Laparoscopic Surgery. Obstet Gynecol Surg (2021) 76(12):751–9. 10.1097/OGX.0000000000000961
4.
Karampinis I Lion E Grilli M Hetjens S Weiss C Vassilev G et al Trocar Site Hernias in Bariatric Surgery-An Underestimated Issue: a Qualitative Systematic Review and Meta-Analysis. Obes Surg (2019) 29(3):1049–57. 10.1007/s11695-018-03687-2
5.
Christie MC Manger JP Khiyami AM Ornan AA Wheeler KM Schenkman NS . Occult Radiographically Evident Port-Site Hernia after Robot-Assisted Urologic Surgery: Incidence and Risk Factors. J Endourol (2016) 30(1):92–6. 10.1089/end.2015.0431
6.
Ciscar A Badia JM Novell F Bolívar S Mans E . Incidence and Risk Factors for Trocar-Site Incisional Hernia Detected by Clinical and Ultrasound Examination: a Prospective Observational Study. BMC Surg (2020) 20(1):330. 10.1186/s12893-020-01000-6
7.
Üstünyurt E Taşgöz FM Tiğrak S . Asymptomatic Trocar Site Hernias: An Underestimated Complication of Laparoscopy. Turk J Obstet Gynecol (2020) 17(3):202–8. 10.4274/tjod.galenos.2020.70952
8.
Karampinis I Lion E Hetjens S Vassilev G Galata C Reissfelder C et al Trocar Site HERnias after Bariatric Laparoscopic Surgery (HERBALS): a Prospective Cohort Study. Obes Surg (2020) 30(5):1820–6. 10.1007/s11695-020-04400-y
9.
Rossi A McLaughlin D Witte S LynSue J Haluck RS Rogers AM . An Expanded Retrospective Review of Trocar Site Hernias in Laparoscopic Gastric Bypass Patients. J Laparoendosc Adv Surg Tech A (2017) 27(6):633–5. 10.1089/lap.2016.0483
10.
Erdas E Dazzi C Secchi F Aresu S Pitzalis A Barbarossa M et al Incidence and Risk Factors for Trocar Site Hernia Following Laparoscopic Cholecystectomy: a Long-Term Follow-Up Study. Hernia (2012) 16(4):431–7. 10.1007/s10029-012-0929-y
11.
Cybulska P Schiavone MB Sawyer B Gardner GJ Zivanovic O Brown CL et al Trocar Site Hernia Development in Patients Undergoing Robotically Assisted or Standard Laparoscopic Staging Surgery for Endometrial Cancer. Gynecol Oncol (2017) 147(2):371–4. 10.1016/j.ygyno.2017.09.005
12.
Nofal MN Ali Jad Yousef AJ Hamdan FF Oudat AH . Characteristics of Trocar Site Hernia after Laparoscopic Cholecystectomy. Sci Rep (2020) 10(1):2868. 10.1038/s41598-020-59721-w
13.
Harriott CB Dreifuss NH Schlottmann F Sadava EE . Incidence and Risk Factors for Umbilical Trocar Site Hernia after Laparoscopic TAPP Repair. A Single High-Volume center Experience. Surg Endosc (2021) 35(9):5167–72. 10.1007/s00464-020-08007-3
14.
Hernandez SM Kiselak EA Zielonka T Tucker S Blatt M Perez JM et al Umbilical Fascial Defects Are Common and Predict Trocar Site Hernias after Laparoscopic Appendectomy. Am Surg (2021). 3134821995063. 10.1177/0003134821995063
15.
Cano-Valderrama O Sanz-López R Sanz-Ortega G Anula R Romera JL Rojo M et al Trocar-site Incisional Hernia after Laparoscopic Colorectal Surgery: a Significant Problem? Incidence and Risk Factors from a Single-center Cohort. Surg Endosc (2021) 35(6):2907–13. 10.1007/s00464-020-07729-8
16.
Gutierrez M Stuparich M Behbehani S Nahas S . Does Closure of Fascia, Type, and Location of Trocar Influence Occurrence of Port Site Hernias? A Literature Review. Surg Endosc (2020) 34(12):5250–8. 10.1007/s00464-020-07826-8
17.
Ahlqvist S Edling A Alm M Dackhammar JB Nordin P Cengiz Y . Trocar Site Hernia after Gastric Sleeve. Surg Endosc (2022) 36(6):4386–91. 10.1007/s00464-021-08787-2
18.
Deerenberg EB Nadia A Henriksen NA Antoniou GA Antoniou SA Bramer WM Fischer JP et al Updated Guideline for Closure of Abdominal wall Incisions from the European and American Hernia Societies. Br J Surg (2022) 109:1239–50. 10.1093/bjs/znac302
19.
Kaistha S Kumar A Gangavatiker R Br S Sisodiya N . Laparoscopic Access: Direct Trocar Insertion versus Open Technique. J Laparoendosc Adv Surg Tech A (2019) 29(4):489–94. 10.1089/lap.2018.0408
20.
Sikar HE Çetin K Eyvaz K Altin O Kaya S Gökçeimam M et al Lateral Sided Trocar Site Hernia Following Laparoscopic Hernia Repair: Results of a Long-Term Follow-Up. Hernia (2019) 23(1):101–6. 10.1007/s10029-018-1864-3
21.
Paasch C Mantke A Hunger R Mantke R . Bladed and Bladeless Conical Trocars Do Not Differ in Terms of Caused Fascial Defect Size in a Porcine Model. Surg Endosc (2022) 36:9179–85. 10.1007/s00464-022-09401-9
22.
Damani T James L Fisher JC Shah PC . Incidence of Acute Postoperative Robotic Port-Site Hernias: Results from a High-Volume Multispecialty center. J Robot Surg (2021) 15(3):457–63. 10.1007/s11701-020-01128-w
23.
Diez-Barroso R Jr Palacio CH Martinez JA Makris K Massarweh NN Chai CY et al Robotic Port-Site Hernias after General Surgical Procedures. J Surg Res (2018) 230:7–12. 10.1016/j.jss.2018.04.032
24.
Pereira N Hutchinson AP Irani M Chung ER Lekovich JP Chung PH et al 5-millimeter Trocar-Site Hernias after Laparoscopy Requiring Surgical Repair. J Minim Invasive Gynecol (2016) 23(4):505–11. 10.1016/j.jmig.2016.03.001
25.
Sun N Zhang J Zhang C Shi Y . Single-site Robotic Cholecystectomy versus Multi-Port Laparoscopic Cholecystectomy: A Systematic Review and Meta-Analysis. Am J Surg (2018) 216(6):1205–11. 10.1016/j.amjsurg.2018.04.018
26.
Antoniou SA García-Alamino JM Hajibandeh S Hajibandeh S Weitzendorfer M Muysoms FE et al Single-incision Surgery Trocar-Site Hernia: an Updated Systematic Review Meta-Analysis with Trial Sequential Analysis by the Minimally Invasive Surgery Synthesis of Interventions Outcomes Network (MISSION). Surg Endosc (2018) 32(1):14–23. 10.1007/s00464-017-5717-4
27.
Christoffersen MW Brandt E Oehlenschläger J Rosenberg J Helgstrand F Jørgensen LN et al No Difference in Incidence of Port-Site Hernia and Chronic Pain after Single-Incision Laparoscopic Cholecystectomy versus Conventional Laparoscopic Cholecystectomy: a Nationwide Prospective, Matched Cohort Study. Surg Endosc (2015) 29(11):3239–45. 10.1007/s00464-015-4066-4
28.
Cisano C Sapienza P Crocetti D de Toma G . Z-Entry Technique Reduces the Risk of Trocar-Site Hernias in Obese Patients. Ann R Coll Surg Engl (2016) 98(5):340–1. 10.1308/rcsann.2016.0114
29.
Omar I Miller K Madhok B Amr B Singhal R Graham Y et al The First International Delphi Consensus Statement on Laparoscopic Gastrointestinal Surgery. Int J Surg (2022) 104:106766. 10.1016/j.ijsu.2022.106766
30.
Wells A Germanos GJ Salemi JL Mikhail E . Laparoscopic Surgeons' Perspectives on Risk Factors for and Prophylaxis of Trocar Site Hernias: A Multispecialty National Survey. JSLS (2019) 23(2). e2019.00013. 10.4293/JSLS.2019.00013
31.
Ece I Yilmaz H Alptekin H Yormaz S Colak B Sahin M . Port Site Hernia after Laparoscopic Sleeve Gastrectomy: a Retrospective Cohort Study of 352 Patients. Updates Surg (2018) 70(1):91–5. 10.1007/s13304-017-0501-5
32.
Rebibo L Demouron M Dembinski J Dhahri A Yzet T Regimbeau J-M . Impact of Routine 12 Mm Epigastric Trocar Site Closure on Incisional Hernia after Sleeve Gastrectomy: a Prospective Before/After Study. Obes Surg (2019) 29(11):3500–7. 10.1007/s11695-019-03971-9
33.
Mikhail E Hart S . Laparoscopic Port Closure. Surg Technol Int (2014) 24:27–33.
34.
Wani AA Khuroo S Jain SK Heer VK Rajput D Maqsood S . The "Flip-Flap" Technique for Laparoscopic Port-Site Closure-Description of a Novel, Cost-Effective Technique with Review of Literature. Surg J (N Y) (2021) 7(3):e168–e171. 10.1055/s-0041-1731270
35.
Lasheen AE Salem A Elaal SA Elsheweal AE Osman G Alkilany M et al Percutaneous Trans-abdominal External Looped Needle with Two Holes in the Trocar Sheath for Port-Site Closures in Difficult Obese Cases. Asian J Endosc Surg (2016) 9(4):295–9. 10.1111/ases.12302
36.
Iranmanesh P Rivera AR Bajwa KS Alibhai M Snyder BE Wilson TD et al Trocar Site Closure with a Novel Anchor-Based (neoClose ®) System versus Standard Suture Closure: a Prospective Randomized Controlled Trial. Surg Endosc (2020) 34(3):1270–6. 10.1007/s00464-019-06891-y
37.
Selvaraj N Dholakia K Ramani S Ragavan N . The Chennai Port Closure Method: A Novel Simple Technique for Laparoscopic Port Closure. Surg Open Sci (2021) 4:37–40. 10.1016/j.sopen.2021.02.001
38.
Takemoto Y Ikeda M Karakuchi N Shimomura M Inoue M Ohmori I et al A Safe and Reliable Technique for Fascial Closure without Special Devices after Laparoscopic Surgery. Asian J Endosc Surg (2021) 14(1):149–53. 10.1111/ases.12809
39.
Kimura M Eguchi Y Kuwabara Y Mitsui A Nagasaki T Nakaya S et al A Simple and Reliable Procedure for Laparoscopic Port-Site Closure. Langenbecks Arch Surg (2021) 406(4):1233–7. 10.1007/s00423-021-02121-z
40.
Donmez T Ozcevik H Sunamak O Yildirim D . Efficacy and Reliability of the Use of a Needle Grasper to Prevent Trocar Site Hernia. Wideochir Inne Tech Maloinwazyjne (2018) 13(4):477–84. 10.5114/wiitm.2018.75867
41.
Tavassoli A Bagheri R Feizzadeh B Tavassoli F Barekati N . Fascial Repair of Laparoscopic Ports with Allis-Hemostat Technique. Indian J Surg (2015) 77(2):245–7. 10.1007/s12262-012-0784-1
42.
Kawai H Misawa T Sasaya K Aoyama Y . Dual-hemostat Port Closure Technique with Customized Surgical Suture after Laparoscopic Cholecystectomy: Single-center Experience. Asian J Endosc Surg (2020) 13(1):83–8. 10.1111/ases.12690
43.
Moreno-Egea A . How to Prevent Trocar-Site Hernia? A Totally Atraumatic Endoscopic Mini-IPOM-Plug Technique (With Extra-lightweight Titanium-Coated Mesh and Glue). Surg Laparosc Endosc Percutan Tech (2015) 25(3):e106–8. 10.1097/SLE.0000000000000153
44.
Armañanzas L Ruiz-Tovar J Arroyo A García-Peche P Armañanzas E Diez M et al Prophylactic Mesh vs Suture in the Closure of the Umbilical Trocar Site after Laparoscopic Cholecystectomy in High-Risk Patients for Incisional Hernia. A Randomized Clinical Trial. J Am Coll Surg (2014) 218(5):960–8. 10.1016/j.jamcollsurg.2014.01.049
45.
Tranchart H Gaillard M Bekkhoucha S Dammaro C Schoucair N Lainas P et al Prevention of Incisional Hernia after Single-Port Sleeve Gastrectomy (PRISM): a Prospective Non-randomized Controlled Study. Surg Endosc (2022) 36:7225–32. 10.1007/s00464-022-09088-y
46.
Abu Gazala M Brodie R Yuval JB Kornblau G Neustadter D Mintz Y . Sutureless Energy-Based Wound Closure: a Step in the Quest for Trocar Site Hernia Prevention. Minim Invasive Ther Allied Technol (2022) 31(4):567–72. 10.1080/13645706.2021.1871630
Summary
Keywords
trocar site, port site, incisional, hernia, prevention
Citation
de Beaux AC and East B (2022) Thoughts on Trocar Site Hernia Prevention. A Narrative Review. J. Abdom. Wall Surg. 1:11034. doi: 10.3389/jaws.2022.11034
Received
06 November 2022
Accepted
09 December 2022
Published
21 December 2022
Volume
1 - 2022
Updates
Copyright
© 2022 de Beaux and East.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: A. C. de Beaux, adebeaux@doctors.org.uk
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.