Abstract
Background: Cervical dystonia impacts quality of life and activities of daily living. Botulinum toxin injections, the standard treatment, are not effective for all and often include bouts of recurring symptoms between injections. There is a need for supplementary treatments such as yoga, which has been shown to be beneficial for individuals with chronic neck pain and movement disorders. However, individuals with cervical dystonia experience barriers impeding access to in-person yoga. Thus, alternative delivery methods that can optimize access while maintaining safety must be investigated. The purpose of this study is to investigate the feasibility and safety of a synchronous one-on-one tele-yoga intervention for individuals with cervical dystonia.
Methods: Individuals with cervical dystonia were enrolled in a single group pilot feasibility study consisting of a 6-weeks tele-yoga intervention bookended by two assessment sessions, ending with a 6-weeks follow-up period and associated final assessment session. The live one-on-one tele-yoga intervention consisted of breathing, postures, and relaxation and was delivered for 30 min twice weekly. Primary outcomes included adherence, adverse events, technological challenges, and usability. Secondary outcomes included enjoyment, yoga status at follow-up, clinically relevant questionnaires, and functional measures.
Results: Of the fifteen individuals enrolled, one did not complete the follow-up assessment. Intervention adherence was 93%. No significant adverse events related to the intervention occurred. Manageable technological challenges occurred. Mean usability and enjoyment were high.
Conclusions: The implementation of a one-on-one tele-yoga intervention for individuals with cervical dystonia is safe and feasible thus, efficacy trials should be initiated.
Clinical Trial Registration: https://www.clinicaltrials.gov/ct2/show/NCT04348669, NCT04348669
Introduction
Cervical dystonia (CD), the most common form of adult-onset focal dystonia, is vastly understudied. With an approximate prevalence of 28–183 cases per million (1), CD is characterized by its cardinal motor impairments including abnormal head and neck posture, decreased range of motion, tremor, and muscle spasms (2). Additionally, individuals with CD often experience comorbid mental health conditions such as symptoms of anxiety, depression, and/or sleep dysfunction (3). Pain, in combination with these non-motor symptoms, often leads to decreased quality of life (3). The current gold standard treatment of botulinum toxin injections (4) focuses primarily on improving motor impairments (5) and pain (6). Additionally, this treatment, while generally safe and effective, often includes bouts of recurring symptoms between injections (7) with decreased satisfaction of treatment occurring prior to reinjections (7). In a survey, out of 1,071 respondents, 25% reported being fairly/very dissatisfied with their care (8). Of 400 respondents who were specifically dissatisfied with their botulinum toxin treatment, 46% reported it was due to non-responsiveness and 33% reported it was due to side effects (8). Thus, there is a need for safe supplementary interventions that can be paired with botulinum-toxin injections and have the potential to address both motor and non-motor impairments of CD while having minimal side effects.
Yoga has the potential to impact both motor and non-motor impairments and has been sought out by individuals with chronic health conditions to manage care (9). Yoga, which can be low impact, may be especially useful for individuals with CD, who report that fatigue and motor symptoms impede participation in physical activity (10). While, to our knowledge, there is no published research involving the implementation of yoga for individuals with CD, yoga has been shown to be beneficial for individuals with chronic neck pain (11) and for others with movement disorders, such as those with Parkinson’s disease (PD) (12–15).
Despite potential benefits of yoga, barriers may make in-person yoga inaccessible for individuals with chronic conditions such as CD. Disease-related mobility impairments make travel to in-person interventions challenging (10). Even if mobility impairments do not impede travel, transportation difficulties including lack of access to a vehicle, distance to the intervention, and costliness of transportation may impede access (16). Individuals with CD also report that a lack of reachable knowledgeable professionals inhibits participation (10). Stigma (10) and the fear of being watched by others may also impede participation in community based in-person yoga classes. Therefore, there is a need for an intervention delivery method that can address these barriers by limiting the need for travel, facilitating access to knowledgeable professionals, and providing the opportunity to engage in interventions in a judgement free environment such as one’s own home.
Delivering yoga remotely via technological means (tele-yoga) may address some of these barriers. Tele-yoga, similarly, to telemedicine and telerehabilitation, can be delivered synchronously (in real-time) or asynchronously (through prerecorded materials). Telemedicine has been used successfully for the evaluation of individuals with CD (17). There is currently an interest in telerehabilitation approaches for this population as indicated in a recently published paper demonstrating telerehabilitation exercises for individuals with CD (18). There is, however, support in the literature for both synchronous and asynchronous tele-interventions for individuals with other movement disorders such as PD (19–21). The work thus far has shown that physical tele-interventions may be safe and beneficial for individuals with PD, however there is less known about other movement disorder populations and tele-yoga specifically.
There are currently no tele-yoga studies specifically investigating individuals with movement disorders, but there is a small body of work regarding tele-yoga in general. Overall, the existing studies consist primarily of asynchronous delivery with a few studies examining synchronous delivery of tele-yoga. However, synchronous tele-yoga may afford opportunities to optimize safety, symptom assessment/management, and participant understanding. Three studies to date have addressed the implementation of synchronous tele-yoga in adult populations, including women with breast cancer (22), individuals with cardiopulmonary conditions (23), and veterans (24). These few existing studies showed high enjoyment, satisfaction, and improvement in mental health outcomes (22–25). Despite potential benefits, the literature is sparse, not specific to CD, and presents some current challenges including technological difficulties and low adherence (22, 23) which may be addressed through changes in the technology used and different approaches to scheduling. This current study aims to build on existing literature by investigating the feasibility and safety of a synchronous one-on-one tele-yoga intervention for individuals with CD. Based on the available literature, we hypothesized that the synchronous tele-yoga intervention would be feasible and safe for individuals with CD.
Materials and Methods
This study was a non-randomized single-group pilot intervention study. It was completed entirely remotely from participants’ residences through videoconferencing (April 2020 and May 2021). It was unblinded and consisted of: 1) baseline assessment session, 2) 6-weeks synchronous tele-yoga intervention period (participants completed twice weekly live yoga sessions one-on-one with a certified instructor), 3) post-intervention assessment session, 4) 6-weeks follow-up period (participants continued their regular activities with no interaction from the study team), and 5) final follow-up assessment session (see Figure 1). This study was registered with ClinicalTrials.gov (NCT04348669) and approved by the Institutional Review Board at Rutgers University. It was reported in accordance with the STROBE guidelines for Cohort Studies (26), and the CONSORT extension for pilot and feasibility trials (27).
FIGURE 1
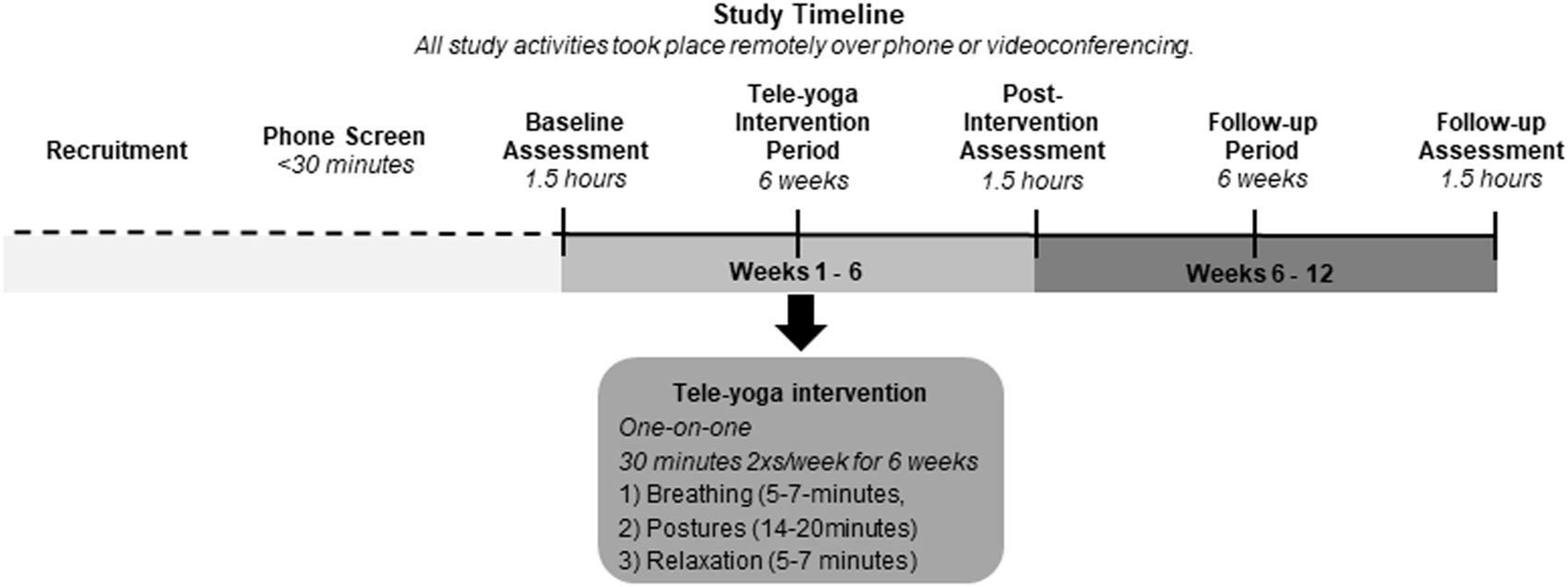
Illustration of the study timeline.
Participants
A convenience sample of 15 individuals with CD were recruited using a study information flyer circulated on online platforms including dystonia-related social media support groups and dystonia-related organization websites. Recruitment ceased when sufficient information regarding feasibility and safety was obtained from enrolled participants. Eligibility was assessed during a phone screen. Individuals were eligible to participate if they were 1) ≥18 years old, 2) English-speaking, 3) diagnosed with CD, 4) able to communicate with the study team and yoga instructor such that they could indicate pain, answer questions, and provide feedback either verbally or through written communication and body gestures, 5) able to access WiFi via an applicable technological device, and 6) agreeable to use Zoom and to be video recorded. People were not eligible if they had 1) unmanaged major depressive disorder (self-reported), 2) a condition that could prevent the ability to engage in physical activity, 3) major cognitive impairment, 4) past yoga experience of five or more times within the last 2 months or 5) were pregnant (self-report). During the first live videoconferencing assessment session eligibility was confirmed and informed consent was obtained.
Intervention
The tele-yoga intervention was delivered to participants’ residences by a certified yoga instructor remotely and synchronously through the videoconferencing platform Zoom individually for 30-min two times a week for 6-weeks. The intervention was developed using the previously published “eight domains for developing a yoga protocol” (28). Each session included three key yogic elements in the following sequence 1) breathing exercises (5–7 min), 2) yoga postures (14–20 min), and 3) meditation exercises (5–7 min). Postures included seated, supine, quadruped, standing postures, and mindful movement of the head and neck depending on the participants’ abilities. The intervention was delivered and modified in real-time to fit the needs of each participant.
Outcome Measures
Primary outcome measures included recruitment rate, retention rate, adherence, adverse events, technological challenges, and usability. Recruitment rate was calculated by computing the number of participants who met the inclusion criteria and were enrolled in the study compared to the number of individuals who engaged in the phone screening process. Retention rate was calculated by computing the number of participants who completed the study compared to those who were enrolled. Adherence was measured via yoga session and assessment session attendance. Adverse events were recorded with their potential relationship to the study and their severity. For technological challenges, anything perceived as a challenge by the yoga instructor or participant was documented with severity of the challenge measured by time disrupted as mild (1–3 min), moderate (3–10 min), or severe (>10 min). Usability was assessed using the ten item Systems Usability Scale (SUS) (29).
Secondary outcome measures included enjoyment, yoga status at follow-up, clinically relevant questionnaires, and functional measures. Enjoyment of the intervention was assessed using a 0–10-point scale for the overall study experience, the overall yoga intervention, and the three yogic elements (breathing, postures, and relaxation/meditation). At the follow-up assessment, participants completed a questionnaire about their yoga practice over the 6-weeks follow-up period after the synchronous tele-yoga intervention had ended. Disease-specific quality of life was assessed by the Craniocervical Dystonia Questionnaire (CDQ-24) (30). General quality of life was assessed with the SF-36 (31). Anxiety and depression were assessed using the Beck Anxiety Inventory (BAI) (32) and Beck Depression Inventory-II (BDI) (33). respectively. Sleep dysfunction was assessed using the Pittsburgh Sleep Quality Index (PSQI) (34). Dystonia symptom severity, disability, and pain were assessed using the Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS) (35). The TWSTRS was administered in real-time over videoconferencing. The session was video recorded and the TWSTRS was scored at a later date using the recorded session. It has been shown that there is excellent agreement between the TWSTRS motor severity domain when it is administered in-person vs. when it is administered during a telemedicine evaluation (17). Lastly, physical function was assessed using the five times sit to stand (FTSTS) (36). Permission and licenses were obtained for questionnaires as applicable.
Data and Statistical Analyses
Score computation and statistical analysis was completed using R and R studio (37, 38). Total scores and available subscale scores were computed for all applicable outcome measures. Missing items were addressed using item mean imputation (i.e., the mean of the specific missing item for the relevant time period across all subjects). Descriptive statistics of all outcomes were calculated. For the relevant clinical outcome measures with normal distributions, repeated measures ANOVAs were computed, and effect sizes (partial eta squared) were calculated. For the relevant clinical outcome measures with non-normal distribution, Friedman tests were computed, and effect sizes (Kendall’s W) were calculated. A secondary analysis was completed in which participants who had received botulinum toxin injections over the course of the study (participants 6, 8, 11, 13, 14, and 15) were excluded from analysis. The methods for the secondary analysis were the same as those for the primary analysis described above.
Results
Of the 67 participants who contacted the study team, 15 participants were enrolled in the study, 14 of which completed the study in its entirety (see Figure 2). Individuals were able to remotely participate from all over the world including Australia (n = 5), Canada (n = 2), and the United States (n = 8). See Table 1 for participant characteristics. Supplementary management techniques for CD symptoms at baseline included: oral pharmaceutical management (n = 5), deep brain stimulation (n = 2), physical activity (n = 7), hypnosis therapy (n = 1), and Bowen therapy (n = 1).
FIGURE 2
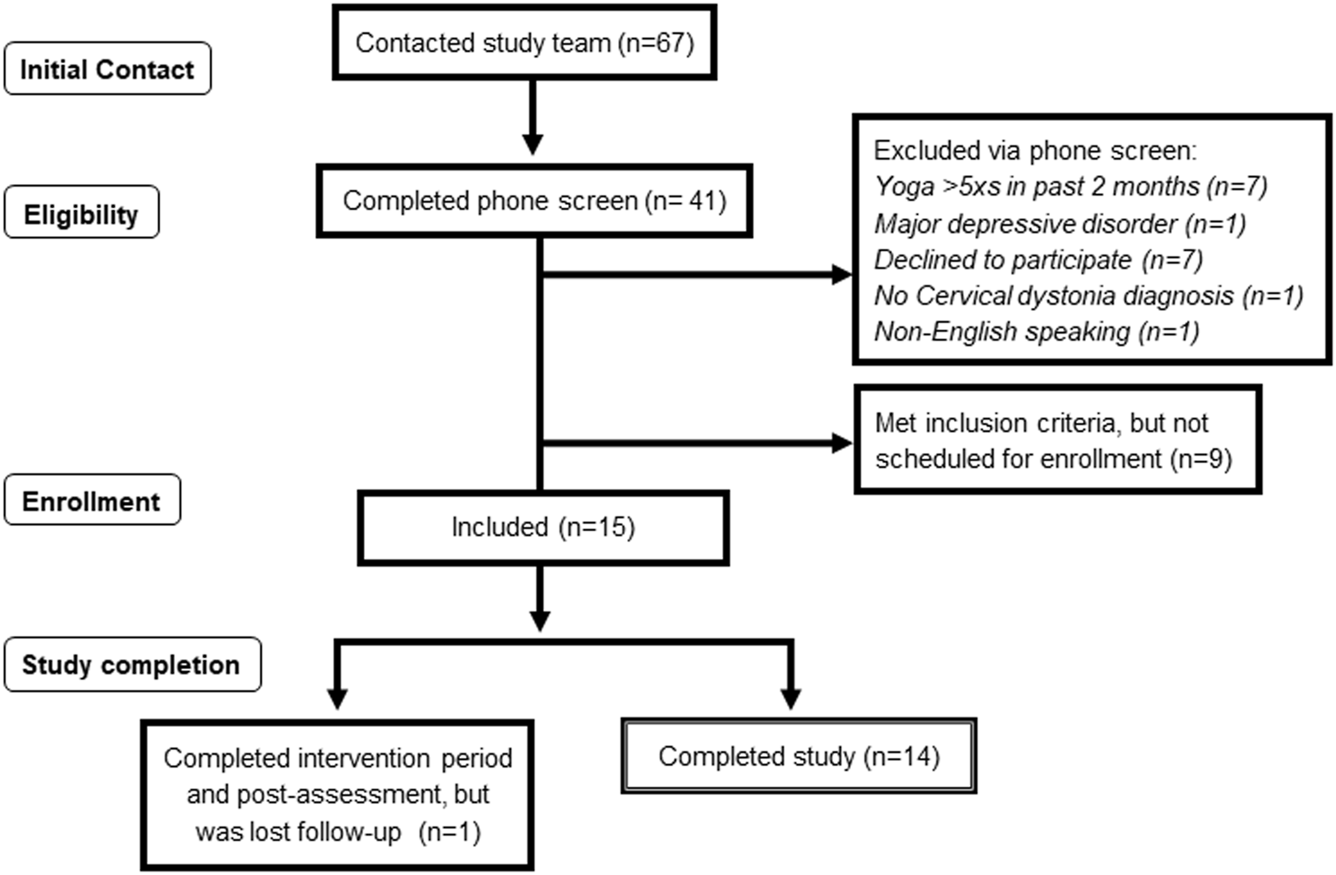
The recruitment and enrollment CONSORT chart.
TABLE 1
| Sex | Female (n = 11), Male (n = 4) |
|---|---|
| Age | 51.13 years ± 13.55 |
| Race | White (n = 14), Bangla (n = 1) |
| Weight | 168.11 lbs ± 38.68 |
| Height | 67.13 in. ± 3.76 |
| Body Mass index | 25.86 ± 4.23 |
| Years since diagnosis | 9.03 ± 8.09 |
| Participants managing CD with botulinum toxin | n = 10 |
Participant demographics.
Abbreviations: CD, cervical dystonia.
Participants 1 and 2 were overdue for botulinum toxin injections at the start of the study by 5 and 2 months, respectively. Due to the pandemic, they did not receive any injections over the course of the study. Participant 11 was 1 month overdue and received a botulinum toxin injection between the first and second yoga session. Participant 15 received a botulinum toxin injection between yoga sessions five and six and was 1 week overdue for the injection at that time. Participant 8 received his first botulinum toxin injection between yoga sessions seven and eight. Participant 6 had not received an injection in years (unable to explicitly quantify) and received one during the 3rd week of the follow-up period. Participant 12 received an injection 1 week prior to the baseline assessment. Participant 13 received an injection 2 months prior to the baseline assessment and then between yoga sessions three and four. Participant 14 received an injection between the baseline assessment and the first yoga session. Participant 10 did not report when they received their most recent injection and did not receive any injections during the study period. All other participants (participants 3, 4, 5, 7, and 9) did not use botulinum toxin injections to manage CD symptoms.
Adherence
Study adherence was high with 14 out of 15 participants completing all three assessment sessions. Yoga-intervention adherence was also high (93%) with 168 sessions attended out of 180 sessions scheduled. Mean attendance was 11.2 ± 1.86 sessions. Eleven participants received 100% of the intended dosage, two of these participants completed the intended 12 sessions within 7 weeks due to rescheduling. Three participants completed at least 10 of the intended sessions, while only one participant completed less than 10 sessions. Reasons for rescheduling included: resting following botulinum injections (n = 1), migraine (n = 1), participant illness (n = 7), instructor illness (n = 3), instructor internet connectivity (n = 3), participant overslept (n = 1), participant scheduling conflict (n = 6), instructor scheduling conflict (n = 3), participant vacation (n = 3). Reasons for cancelations included unrelated exacerbation of CD (n = 4), instructor power-outage (n = 1), participant no-show with reason not-provided (n = 3), and participant scheduling conflicts (n = 3). Participants were encouraged to engage in home practice between intervention sessions consisting of the exercises taught in each session. Participants reported engaging in home practice inconsistently and were generally unable to quantify or specify what they did.
Safety
No significant adverse events were attributed to the intervention. As expected, all participants reported baseline pain including CD-related (neck/shoulder) pain (n = 15), hip pain (n = 3), low back pain (n = 3), and ankle pain (n = 1). Seven participants reported temporary increases in pain (one-point) during specific postures. At the end of one session a participant reported a one-point pain increase, but resolved the pain through self-massage. Other mild events related to the intervention included transient dizziness with a position change (n = 1), headache following a position change (n = 1), as well as temporary increases in symptoms in supine position (n = 1) and with breathing exercises (n = 1); all of which abated when the activities were stopped. Five events (resulting in modification of the yoga sessions) with a possible causal relationship to the intervention included development of new soreness/pulling at the shoulders (n = 2), increased rigidity/soreness of the back of the neck (n = 1), new hip pain (n = 1), and new low back pain (n = 1) during the course of the intervention, all of which resolved prior to the end of the study. Two participants reported transient mood fluctuations, one unrelated between sessions, and one during the relaxation exercises which resolved prior to the session’s end. Mild unrelated events were successfully managed by participants and/or their neurologists as applicable. These mild unrelated events included injection site pain following botulinum toxin injections (n = 1), increased whole body shaking attributed to a medication error (n = 1), and chest tightness attributed to asthma (n = 1). One moderate event unrelated to the intervention (mild symptoms of the Sars-CoV-2 virus) resulted in the rescheduling of one session. Lastly, one severe unrelated event occurred during the follow-up period in which a participant was hospitalized for differential diagnosis of an occipital migraine.
Technological Challenges
Various technological challenges occurred during the yoga sessions (Table 2). Audio and visual delays, the most common challenge, did not greatly disrupt time but did impact session quality. A few mild interruptions not caused by technological challenges disrupted time from the study. None of the mild or moderate challenges/interruptions impacted the amount of yoga received, as time disruption was accommodated within affected sessions. Most severe challenges were also able to be accommodated. However, in two instances, the instructor had difficulty connecting to the internet and needed to reschedule the sessions. Despite these technological challenges, scores on the SUS (89.67 ± 7.67) indicated good usability.
TABLE 2
| Mild (1–3 min) | Moderate (3–10 min) | Severe (>10 min) | |
|---|---|---|---|
| Audio challenges | -Difficulty hearing speaker (n = 4) | None | -Volume on low (n = 1) |
| -Unable to connect to audio (n = 1) | -Unable to connect to audio (n = 1) | ||
| Video challenges | -One screen freeze (n = 2) | None | -Difficulty turning on video (n = 1) |
| -Screen freeze + video reboot (n = 1) | |||
| -Recurring screen freezing (n = 1) | |||
| Audio/video delay | (27 sessions) | None | None |
| Difficulty logging in | -Received incorrect link (n = 1) | -Unable to exit waiting room into session (n = 1) | -Participant stuck in waiting room, instructor unaware (n = 1) |
| - Participant wanted to change devices (n = 1) | |||
| Disruptions | -Misc. interruptions (cause unknown) (n = 3) | -Computer updated (n = 1) | None |
| -People in the house (n = 3) | |||
| -Phone alarm (n = 1) | |||
| Internet connectivity | -Dropped call(s) (One/session n = 10, two/session n = 1) | - Difficulty connecting to internet (n = 3) | -Difficulty connecting to internet (n = 3) |
| - Dropped call(s) (one/session n = 2, two/session n = 1, nine/session n = 1) |
Technological challenges during yoga sessions.
Enjoyment and Yoga Status at Follow-Up
Mean enjoyment scores were high for the remote study experience (9.5 ± 0.94), overall yoga intervention (9.2 ± 1.37), breathing exercises (8.6 ± 2.61), postures (9.07 ± 1.22), and relaxation exercises (8.73 ± 2.25). Despite high enjoyment levels, not all participants continued to practice yoga consistently after the intervention period ended during the 6-weeks follow-up period. Participants reported varying levels of practice including inconsistent practice (n = 5), one time per week (n = 1), two-three times per week (n = 4), and greater than three times per week (n = 4). Participants reported practicing at home without any instruction (n = 11), via live videoconferencing (n = 2), and through online videos (n = 1). Participants reported practicing postures, breathing, and meditation (n = 8), postures and breathing (n = 3), postures and meditation (n = 1), and meditation only (n = 1). Two participants reported not practicing as much as they desired because they did not have access to an instructor while another attributed lack of practice to low energy levels.
Clinically Relevant Measures
There were 10, 4, and 140 items missing for the baseline, post-intervention, and follow-up assessment periods respectively (Supplementary Table S1). Overall disease related quality of life and the subdomains of stigma and emotional well-being demonstrated preliminary efficacy with post-hoc testing indicating significant differences between the baseline and post-assessment periods for these measures. In addition to disease-related quality of life, statistically significant improvements were also seen in CD severity as shown by the severity subscale on the TWSTRS, with post-hoc testing revealing improvements between baseline and post intervention. No other outcomes demonstrated statistically significant differences. See Table 3 and Supplementary Table S2 for detailed results, including effect sizes which ranged from small to large. See Figures 3, 4 for a visual representation of the total scores for the CDQ-24 and TWSTRS, respectively. Additionally, a supplementary analysis of the data, excluding all participants who received a botulinum toxin injection was also performed to minimize the possibility that the improvements observed here were solely related to the effect of the injection in those participants. While minor differences were observed in the magnitude of the effect sizes across the different outcome measures, statistically significant differences remained for the CDQ-24 total score, stigma subscale, and emotional wellbeing subscale as well as for the TWSTRS symptom severity subscale. An additional statistically significant difference also emerged for the SF-36 general health subscale. Detailed results of this secondary analysis can be found in the Supplementary Tables S3, S4 as well as Supplementary Figures S1, S2.
TABLE 3
| Outcome | Baseline (n = 15) | Post (n = 15) | Follow-up (n = 15α) | Effect size | |
|---|---|---|---|---|---|
| (mean ± sd) | (mean ± sd) | (mean ± sd) | ηP2 (for normal distribution) | ||
| W (for non-normal distribution) | |||||
| CDQ-24 | Stigma * | (11.467 ± 6.278) | (7.667 ± 6.253) | (8.600 ± 6.479) | ηP2 = 0.309 |
| Pain | (4.867 ± 3.357) | (3.600 ± 2.324) | (3.467 ± 2.475) | ηP2 = 0.129 | |
| ADLs | (10.600 ± 4.188) | (9.533 ± 3.114) | (10.267 ± 4.183) | W = 0.084 | |
| EWB * | (6.000 ± 3.855) | (3.467 ± 2.800) | (4.133 ± 3.335) | ηP2 = 0.300 | |
| Social | (2.267 ± 2.344) | (1.667 ± 2.267) | (2.600 ± 2.501) | W = 0.0760 | |
| Total * | (35.200 ± 14.304) | (25.933 ± 12.418) | (29.067 ± 14.621) | ηP2 = 0.316 | |
| SF-36 | Physical Funct. | (57.000 ± 16.013) | (56.333 ± 20.131) | (54.000 ± 22.536) | ηP2 = 0.023 |
| RLPH | (31.667 ± 30.570) | (30.000 ± 34.330) | (38.333 ± 37.639) | W = 0.011 | |
| RLEP | (60.000 ± 44.005) | (80.000 ± 37.374) | (71.111 ± 45.192) | W = 0.113 | |
| General | (62.000 ± 22.504) | (56.000 ± 25.579) | (56.667 ± 22.414) | W = 0.106 | |
| Fatigue | (48.667 ± 18.074) | (52.667 ± 17.715) | (47.000 ± 18.107) | ηP2 = 0.127 | |
| Social | (75.000 ± 18.900) | (73.333 ± 21.582) | (65.000 ± 24.640) | ηP2 = 0.079 | |
| Pain | (41.500 ± 28.075) | (52.500 ± 26.271) | (43.333 ± 21.395) | ηP2 = 0.186 | |
| EWB | (68.800 ± 16.984) | (74.133 ± 13.169) | (69.333 ± 16.676) | ηP2 = 0.170 | |
| TWSTRS | Severity * | (18.467 ± 5.097) | (15.867 ± 6.490) | (16.333 ± 5.802) | ηP2 = 0.252 |
| Disability | (14.200 ± 5.570) | (14.933 ± 5.147) | (15.533 ± 5.235) | ηP2 = 0.153 | |
| Pain | (10.583 ± 5.203) | (10.300 ± 4.827) | (11.283 ± 5.148) | ηP2 = 0.060 | |
| Total | (43.250 ± 12.784) | (41.100 ± 14.16) | (43.150 ± 13.817) | ηP2 = 0.066 | |
| PSQI | Quality | (0.933 ± 0.704) | (1.133 ± 0.516) | (1.200 ± 0.561) | W = 0.061 |
| Latency | (1.267 ± 1.100) | (1.133 ± 0.915) | (1.200 ± 1.146) | W = 0.006 | |
| Duration | (0.733 ± 0.884) | (0.933 ± 0.703) | (0.933 ± 1.033) | W = 0.043 | |
| Efficiency | (0.600 ± 0.910) | (0.800 ± 0.94)1 | (1.000 ± 1.195) | W = 0.054 | |
| Disturbance | (1.267 ± 0.704) | (1.000 ± 0.535) | (1.133 ± 0.640) | W = 0.160 | |
| Med. use | (1.333 ± 1.345) | (1.200 ± 1.373) | (0.867 ± 1.366) | W = 0.200 | |
| Daytime Dysf. | (1.000 ± 0.535) | (1.000 ± 0.655) | (0.933 ± 0.800) | W = 0.007 | |
| Total | (7.133 ± 3.962) | (7.200 ± 2.883) | (7.267 ± 3.807) | ηP2 = 0.001 | |
| FTSTS | (13.919 ± 4.066) | (13.617 ± 5.239) | (12.117 ± 2.898) | W = 0.093 | |
| BAI | (11.133 ± 9.782) | (10.400 ± 8.781) | (10.733 ± 9.528) | W = 0.011 | |
| BDI | (8.600 ± 7.772) | (7.333 ± 6.943) | (9.333 ± 8.095) | W = 0.101 | |
Results of relevant clinical and functional outcome measures.
Abbreviations: BAI, beck anxiety inventory; BDI, beck depression inventory; CDQ-24, craniocervical dystonia questionnaire-24, Daytime dysf., daytime dysfunction, EWB, emotional wellbeing; FTSTS, five times sit to stand, Physical funct., physical function, PSQI, pittsburgh sleep quality index; RLEP, role limitations due to emotional problems; RLPH, role limitation due to physical health, and SF-36, 36-Item Short Form Survey Instrument, TWSTRS, toronto western spasmodic torticollis rating scales. Asterisks identify statistically significant differences (p < .05).
FIGURE 3
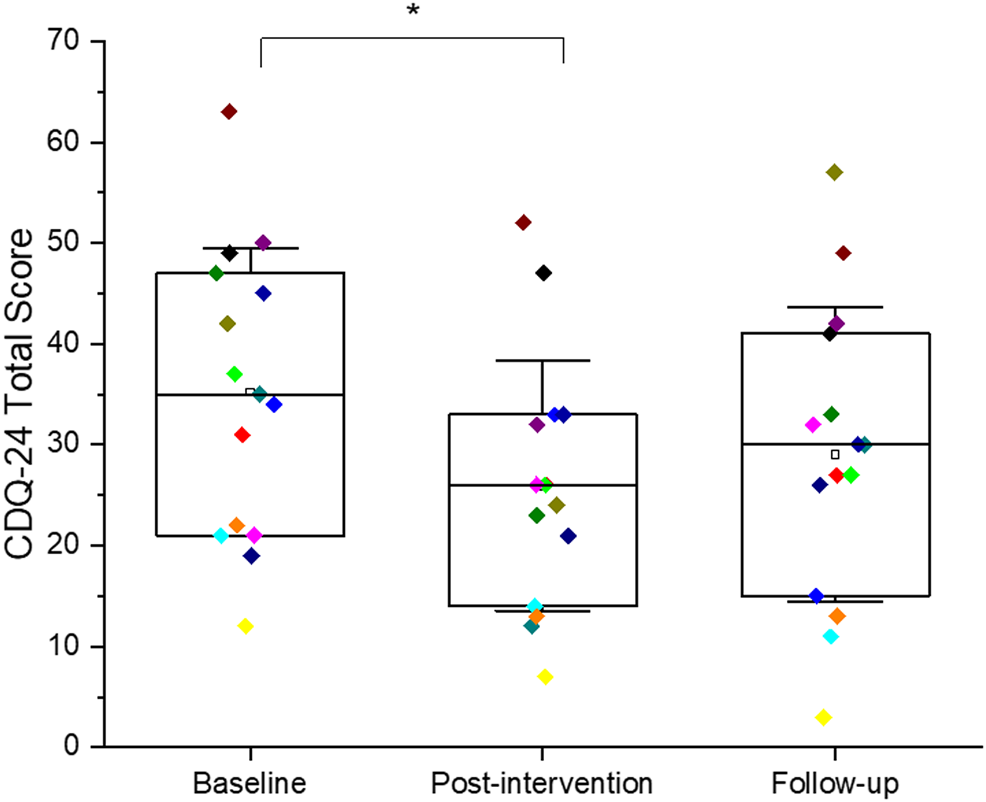
Box plot with individual data points (with a differ color for each participant) for total scores on the CDQ-24 across the three different time points (baseline, post-intervention, and follow-up). The error bars represent one standard deviation. Statistically significant differences (p < 0.05) are indicated with *.
FIGURE 4
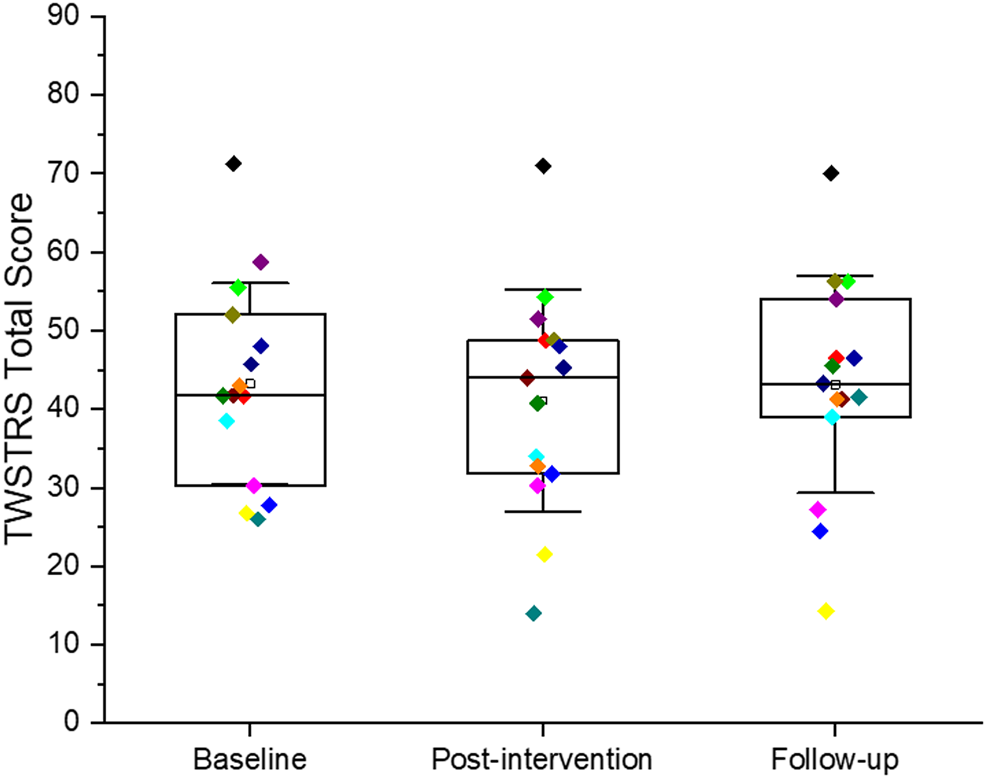
Box plot with individual data points (with a differ color for each participant) for total scores on the TWSTRS across the three different time points (baseline, post-intervention, and follow-up). The error bars represent one standard deviation.
Discussion
To our knowledge this study is the first to establish the feasibility and safety of a tele-yoga intervention for individuals with CD. Notably, it is also one of the few studies investigating a non-pharmaceutical intervention for individuals with CD.
Safety
This study showed that a tele-yoga intervention for individuals with CD is safe, similar to previous findings showing yoga to be generally as safe as other exercise (39). Another synchronous tele-yoga study for individuals with chronic conditions also reported the intervention was safe (23). Asynchronous yoga interventions using pre-recorded videos also reported the interventions to be safe with no significant adverse events (40–42). For individuals with movement disorders such as PD, in-person yoga interventions have also not reported any significant adverse events (13, 43, 44). Thus, our results suggest that, as previously reported, yoga is a safe intervention that can be provided remotely via videoconference.
While no major adverse events occurred, some participants experienced varied one-point increases in pain during specific postures (e.g., side bends, chair posture, forward fold, cat/cow, warrior II, and baby cobra) which attenuated with modification or elimination of the relevant posture. This finding is similar to a yoga study involving individuals with PD who demonstrated knee pain in specific postures which resolved with posture modification (13). This emphasizes the importance of individualization of the yoga intervention. The one-on-one nature of this intervention allowed the instructor to accommodate each participant’s reaction to the postures by modifying postures, slowing the speed of the session, and eliminating specific postures when needed. With these modifications, participants reported that their pain returned to baseline levels within an acceptable time. Future studies should investigate whether this individualized approach is more beneficial than group interventions where personalized feedback and instructors are not always possible.
Feasibility
The current study showed that despite technological challenges, adherence was high and 14 participants achieved 80% or more of the intended dosage. This is in contrast to previous studies demonstrating that technological challenges impeded high adherence. Specifically, previous studies attributed feasibility challenges to scheduling difficulties (22), specific characteristics of the videoconferencing platform used (23), and technological literacy (23). We addressed those challenges by choosing to deliver the intervention individually according to the participant’s availability, and by utilizing a readily available videoconferencing platform with an easy user interface. It must also be noted that this study took place during the Sars-CoV-2 pandemic in which the availability and use of videoconferencing platforms increased significantly. This general global increase in technological literacy may have impacted technological literacy of the participants and may positively impact future tele-rehabilitation studies.
Another factor that may have positively impacted feasibility was that the yoga instructor informed participants that challenges may occur and instructed them on how to navigate them if they arose. Additionally, the instructor modified the yoga sessions to accommodate video/audio delay by speaking in shorter bouts and providing fewer cues, emphasizing safety cues. Only one participant reported that the technological challenges negatively impacted their feelings about the yoga classes.
Interestingly, while intervention adherence was high (93%) and assessment session adherence was also high with only one participant missing the final assessment session, yoga practice over the follow-up period was inconsistent. It is important to note that while participants were strongly encouraged to continue with some type of yoga practice over the 6-weeks follow-up period, similar to what they had completed during the intervention period, they were not explicitly instructed to practice for a set frequency or dosage. Nor were participants provided with any resources such as videos or handouts to practice. This may have contributed to the inconsistency of practice, as some participants noted that they did not practice because they did not have access to an instructor. Future studies could address this by providing a target frequency and dosage for yoga practice during the follow-up as well as by providing participants with practice resources such as videos, handouts, or contact information for other qualified yoga instructors. Implementing these steps may help participant continue the yoga practice after the study has stopped and serve as a stepping-stone for positive behavior change.
Preliminary Efficacy
Interestingly, statistically significant improvements in disease-specific quality of life (i.e., CDQ-24 stigma, emotional well-being, and total score) as well as in motor symptom severity as assessed by the TWSTRS were observed in the current study. Both the primary analysis including all participants and the secondary analysis including only participants who did not receive botulinum toxin injections over the course of the study support these findings. While there is limited information related to complementary therapies for individuals with CD, there appears to be evidence that physical therapy and exercise can lead to improvements in symptom severity (45–49). Other spheres of quality of life and TWSTRS sub-scores also exhibited moderate effect sizes, as supported in both the primary and secondary analyses, such that future studies could be powered to specifically examine the effect of tele-yoga on these clinically important factors. The effect sizes for sleep, physical function, anxiety, and depression were very small in the current study. However, our study sample did not exhibit any significant impairments in those spheres at baseline. Therefore, tele-yoga may still benefit individuals with CD that have those issues but future studies with more targeted inclusion criteria are needed. In fact, yoga has been shown to improve sleep quality (50), physical function (44), anxiety (13, 51), and depression (13, 51) in other populations.
It is important to note that this study did not show any significant improvements in pain either through the TWSTRS or SF-36. Pain is one of the major contributors to poor quality of life in people with CD and is an important symptom to address (52). The findings found here may be attributed to the small sample size as this study was not powered to assess the efficacy of the intervention on pain. Additionally, it is possible that the overall dosage of the intervention was too low to significantly improve pain. It is important to note that several studies in other populations have demonstrated the beneficial effect of yoga practice for pain management (53). Therefore, while the current study did not observe significant improvement in pain, future studies are needed to better establish the efficacy of a tele-yoga intervention on pain in people with CD. Additionally, future studies should also examine the interaction between botulinum toxin injections, which have been shown to significantly reduce pain in people with CD (6), and tele-yoga to identify whether one can potentiate the effect of the other.
Limitations
We acknowledge that this study has limitations. This was a non-randomized, single group, unblinded study with a small sample size. The primary purpose of this study was to assess safety and feasibility across a variety of individuals with CD and, as such, a pragmatic recruitment approach was implemented. Participants were included regardless of disease severity, disease duration, and botulinum injection status. These factors along with other confounding factors such as age and sex were not accounted for in the primary analysis as this was not a primary aim of the study. Yet, despite this heterogeneity in participant characteristics, the intervention was safe and feasible. Future randomized control trials should more specifically address confounding factors either through eligibility criteria or analysis. It is also important to note that while participants were asked to confirm that they had received a diagnosis of CD from a neurologist, this was not corroborated by a physician or with medical documentation. There may also be a selection bias such that individuals comfortable with technology and already engaged in or interested in physical activity may have expressed greater interest in study participation. We also acknowledge that the yoga instructor’s scheduling flexibility along with the Sars CoV-2 pandemic and associated stay at home practices may have positively impacted adherence. Taken together these limitations indicate that results, especially those relating to preliminary efficacy, should be considered cautiously. Nonetheless, the results of this study are encouraging and can be used to power a larger randomized controlled study.
Future Implications
As mentioned, current treatment strategies for individuals with CD focus on alleviating abnormal head postures through botulinum toxin injections but a significant proportion of patients are not satisfied with the outcome of this intervention. Developing tele-rehabilitation approaches that would lead to improved clinical outcomes, greater access to knowledgeable providers, and minimize overall burden could drastically change the prognosis of individuals diagnosed with CD. One could envision a hybrid model of care where patients can get in-person treatment (e.g., botulinum toxin injections) and virtual care with a multi-disciplinary team of physical and occupational therapists, psychologists, and others. To achieve this, future randomized trials informed by the information gathered here are warranted.
Conclusion
This study shows that one-on-one tele-yoga is safe and feasible for individuals with CD. Furthermore, preliminary effectiveness shows statistically significant improvements in quality of life and symptom severity indicating that this complementary approach should be further studied for the management of individuals with CD.
Statements
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: 10.7303/syn25891139 synapse.org.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Board at Rutgers University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
AJ-P participated in the research project conceptualization, methodology, organization, and execution (contacted/screened interested participants, conducted assessment sessions, and implemented intervention sessions); was involved in formal statistical analysis, design, execution, and review/critique; and assisted in writing the first draft of manuscript and reviewing and revising subsequent drafts. J-FD participated in the research project conceptualization, methodology, organization, and execution (supervising and assisting AJ-P) and project administration; was involved in formal statistical analysis design, execution, and review/critique; and co-wrote wrote the first draft of manuscript with AJ-P and supervised/participated in reviewing, editing and revising subsequent drafts.
Funding
The study was internally funded by the Department of Rehabilitation and Movement Sciences of Rutgers University.
Acknowledgments
We thank the participants and their families. We acknowledge Ellen Z. Anderson, Judith E. Deutsch, Carrie Esopenko and Samantha Farris who provided guidance and feedback on study design and implementation. We also thank Shannon Crehan, Miriam Pomerantz, and Sanya Ravoori who assisted in recruitment efforts.
Conflict of interest
J-FD has received funding from NIH, the Michael J. Fox Foundation for Parkinson’s Research, the CIHR, the Weston Brain Institute, the Thrasher Foundation, and from the Reseau Parkinson Quebec. J-FD also has equity in Neuromotrix and Medapplets.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontierspartnerships.org/articles/10.3389/dyst.2021.10015/full#supplementary-material.
References
1.
Defazio G Jankovic J Giel JL Papapetropoulos S . Descriptive Epidemiology of Cervical Dystonia. tre-03-193-4374-2. Tremor Other Hyperkinet Mov (N Y) (2013) 3:3. 10.7916/D80C4TGJ
2.
Albanese A Bhatia K Bressman SB DeLong MR Fahn S Fung VSC et al Phenomenology and Classification of Dystonia: a Consensus Update. Mov Disord (2013) 28(7):863–73. 10.1002/mds.25475
3.
Novaretti N Cunha ALN Bezerra TC Pereira MAP De Oliveira DS Brito MMCM et al The Prevalence and Correlation of Non-motor Symptoms in Adult Patients with Idiopathic Focal or Segmental Dystonia. Tremor Other Hyperkinet Mov (N Y) (2019) 9:596. 10.5334/tohm.466
4.
Contarino MF Van Den Dool J Balash Y Bhatia K Giladi N Koelman JH et al Clinical Practice: Evidence-Based Recommendations for the Treatment of Cervical Dystonia with Botulinum Toxin. Front Neurol (2017) 8:35. 10.3389/fneur.2017.00035
5.
Ravindran K Ganesh Kumar N Englot DJ Wilson TJ Zuckerman SL . Deep Brain Stimulation versus Peripheral Denervation for Cervical Dystonia: A Systematic Review and Meta-Analysis. World Neurosurg (2019) 122:e940–e946. 10.1016/j.wneu.2018.10.178
6.
Camargo C Cattai L Teive H . Pain Relief in Cervical Dystonia with Botulinum Toxin Treatment. Toxins (2015) 7(6):2321–35. 10.3390/toxins7062321
7.
Taylor J Poliziani M Liu X Koch M . Striving for More Good Days: Patient Perspectives on Botulinum Toxin for the Treatment of Cervical Dystonia. Ppa (2016) Vol. 10:1601–8. 10.2147/PPA.S106560
8.
Comella C Bhatia K . An International Survey of Patients with Cervical Dystonia. J Neurol (2015) 262(4):837–48. 10.1007/s00415-014-7586-2
9.
Cramer H Ward L Steel A Lauche R Dobos G Zhang Y . Prevalence, Patterns, and Predictors of Yoga Use. Am J Prev Med (2016) 50(2):230–5. 10.1016/j.amepre.2015.07.037
10.
McCambridge A Meiring RM Bradnam LV . Physical Activity, Sedentary Behavior, and Barriers to Exercise in People Living with Dystonia. Front Neurol (2019) 10:1121. 10.3389/fneur.2019.01121
11.
Li Y Li S Jiang J Yuan S . Effects of Yoga on Patients with Chronic Nonspecific Neck Pain. Medicine (Baltimore) (2019) 98(8):e14649. 10.1097/MD.0000000000014649
12.
Roland K . Applications of Yoga in Parkinson's Disease: a Systematic Literature Review. Jprls (2014) 2014:1. 10.2147/JPRLS.S40800
13.
Kwok JYY Kwan JCY Auyeung M Mok VCT Lau CKY Choi KC et al Effects of Mindfulness Yoga vs Stretching and Resistance Training Exercises on Anxiety and Depression for People with Parkinson Disease. JAMA Neurol (2019) 76(7):755–63. 10.1001/jamaneurol.2019.0534
14.
Van Puymbroeck M Walter A Hawkins BL Sharp JL Woschkolup K Urrea-Mendoza E et al Functional Improvements in Parkinson's Disease Following a Randomized Trial of Yoga. Evidence-Based Complement Altern Med (2018) 2018:1–8. 10.1155/2018/8516351
15.
Jin X Wang L Liu S Zhu L Loprinzi PD Fan X . The Impact of Mind-Body Exercises on Motor Function, Depressive Symptoms, and Quality of Life in Parkinson's Disease: A Systematic Review and Meta-Analysis. Ijerph (2019) 17(1):31. 10.3390/ijerph17010031
16.
Syed ST Gerber BS Sharp LK . Traveling towards Disease: Transportation Barriers to Health Care Access. J Community Health (2013) 38(5):976–93. 10.1007/s10900-013-9681-1
17.
Fraint A Stebbins GT Pal G Comella CL . Reliability, Feasibility and Satisfaction of Telemedicine Evaluations for Cervical Dystonia. J Telemed Telecare (2020) 26(9):560–7. 10.1177/1357633X19853140
18.
Castagna A Saibene E Ramella M . How Do I Rehabilitate Patients with Cervical Dystonia Remotely?Mov Disord Clin Pract (2021) 8(5):820–1. 10.1002/mdc3.13212
19.
Canning CG Sherrington C Lord SR Close JCT Heritier S Heller GZ et al Exercise for Falls Prevention in Parkinson Disease: a Randomized Controlled Trial. Neurology (2015) 84(3):304–12. 10.1212/WNL.0000000000001155
20.
Lai B Bond K Kim Y Barstow B Jovanov E Bickel CS . Exploring the Uptake and Implementation of Tele-Monitored home-exercise Programmes in Adults with Parkinson's Disease: A Mixed-Methods Pilot Study. J Telemed Telecare (2020) 26(1-2):53–63. 10.1177/1357633X18794315
21.
Demartini B Bombieri F Goeta D Gambini O Ricciardi L Tinazzi M . A Physical Therapy Programme for Functional Motor Symptoms: A Telemedicine Pilot Study. Parkinsonism Relat Disord (2020) 76:108–11. 10.1016/j.parkreldis.2019.05.004
22.
Addington EL Sohl SJ Tooze JA Danhauer SC . Convenient and Live Movement (CALM) for Women Undergoing Breast Cancer Treatment: Challenges and Recommendations for Internet-Based Yoga Research. Complement Therapies Med (2018) 37:77–9. 10.1016/j.ctim.2018.02.001
23.
Donesky D Selman L McDermott K Citron T Howie-Esquivel J . Evaluation of the Feasibility of a home-based TeleYoga Intervention in Participants with Both Chronic Obstructive Pulmonary Disease and Heart Failure. J Altern Complement Med (2017) 23(9):713–21. 10.1089/acm.2015.0279
24.
Schulz-Heik RJ Meyer H Mahoney L Stanton MV Cho RH Moore-Downing DP et al Results from a Clinical Yoga Program for Veterans: Yoga via Telehealth Provides Comparable Satisfaction and Health Improvements to In-Person Yoga. BMC Complement Altern Med (2017) 17(1):198. 10.1186/s12906-017-1705-4
25.
Selman L McDermott K Donesky D Citron T Howie-Esquivel J . Appropriateness and Acceptability of a Tele-Yoga Intervention for People with Heart Failure and Chronic Obstructive Pulmonary Disease: Qualitative Findings from a Controlled Pilot Study. BMC Complement Altern Med (2015) 15:21. 10.1186/s12906-015-0540-8
26.
Vandenbroucke JP von Elm E Altman DG Gøtzsche PC Mulrow CD Pocock SJ et al Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. Int J Surg (2014) 12(12):1500–24. 10.1016/j.ijsu.2014.07.014
27.
Eldridge SM Chan CL Campbell MJ Bond CM Hopewell S Thabane L et al CONSORT 2010 Statement: Extension to Randomised Pilot and Feasibility Trials. BMJ (2016) 355:i5239. 10.1136/bmj.i5239
28.
Sherman KJ . Guidelines for Developing Yoga Interventions for Randomized Trials. Evidence-Based Complement Altern Med (2012) 2012:1–16. 10.1155/2012/143271
29.
Lewis JR Sauro J . The Factor Structure of the System Usability Scale. Computer Science (2009) 5619:94–103. 10.1007/978-3-642-02806-9_12
30.
Müller J Wissel J Kemmler G Voller B Bodner T Schneider A et al Craniocervical Dystonia Questionnaire (CDQ-24): Development and Validation of a Disease-specific Quality of Life Instrument. J Neurol Neurosurg Psychiatry (2004) 75(5):749–53. 10.1136/jnnp.2003.013441
31.
Stansfeld SA Roberts R Foot SP . Assessing the Validity of the SF-36 General Health Survey. Qual Life Res (1997) 6(3):217–24. 10.1023/a:1026406620756
32.
Beck AT Epstein N Brown G Steer RA . An Inventory for Measuring Clinical Anxiety: Psychometric Properties. J Consulting Clin Psychol (1988) 56(6):893–7. 10.1037//0022-006x.56.6.893
33.
Wang Y-P Gorenstein C . Psychometric Properties of the Beck Depression Inventory-II: a Comprehensive Review. Rev Bras Psiquiatr (2013) 35(4):416–31. 10.1590/1516-4446-2012-1048
34.
Buysse DJ Reynolds CF 3rd Monk TH Berman SR Kupfer DJ . The Pittsburgh Sleep Quality Index: a New Instrument for Psychiatric Practice and Research. Psychiatry Res (1989) 28(2):193–213. 10.1016/0165-1781(89)90047-4
35.
Boyce MJ Canning CG Mahant N Morris J Latimer J Fung VSC . The Toronto Western Spasmodic Torticollis Rating Scale: Reliability in Neurologists and Physiotherapists. Parkinsonism Relat Disord (2012) 18(5):635–7. 10.1016/j.parkreldis.2012.02.007
36.
Duncan RP Leddy AL Earhart GM . Five Times Sit-To-Stand Test Performance in Parkinson's Disease. Arch Phys Med Rehabil (2011) 92(9):1431–6. 10.1016/j.apmr.2011.04.008
37.
RStudio Team. RStudio: Integrated Development Environment for R (2021). http://www.rstudio.com/, February 2021.
38.
R Core Team. R. A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing (2021). https://www.r-project.org/, February 2021.
39.
Cramer H Ward L Saper R Fishbein D Dobos G Lauche R . The Safety of Yoga: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Am J Epidemiol (2015) 182(4):281–93. 10.1093/aje/kwv071
40.
Stan DL Croghan KA Croghan IT Jenkins SM Sutherland SJ Cheville AL et al Randomized Pilot Trial of Yoga versus Strengthening Exercises in Breast Cancer Survivors with Cancer-Related Fatigue. Support care cancer (2016) 24:4005–15. 10.1007/s00520-016-3233-z
41.
Sakuma Y Sasaki-otomaru A Ishida S Kanoya Y Arakawa C Mochizuki Y et al Effect of a Home-Based Simple Yoga Program in Child-Care Workers: A Randomized Controlled Trial. J Altern Complement Med (2012) 18(8):769–76. 10.1089/acm.2011.0080
42.
Woodside H Culos-Reed SN Grégoire MC Rutledge R Keats MR . Yoga for Young Adults with Noncurative Cancer: A Brief Report. Glob Adv Health Med (2018) 7:2164956118763523. 10.1177/2164956118763523
43.
Justice C Cheung C Samson-Burke A . Development and Evaluation of a Yoga Intervention Program for Parkinson's Disease. Int J Yoga Ther (2018) 28(1):113–22. 10.17761/2018-00015r2
44.
Cheung C Bhimani R Wyman JF Konczak J Zhang L Mishra U et al Effects of Yoga on Oxidative Stress, Motor Function, and Non-motor Symptoms in Parkinson's Disease: a Pilot Randomized Controlled Trial. Pilot Feasibility Stud (2018) 4:162. 10.1186/s40814-018-0355-8
45.
Boyce MJ Canning CG Mahant N Morris J Latimer J Fung VS . Active Exercise for Individuals with Cervical Dystonia: a Pilot Randomized Controlled Trial. Clin Rehabil (2013) 27(3):226–35. 10.1177/0269215512456221
46.
Bradnam LV Meiring RM Boyce M McCambridge A . Neurorehabilitation in Dystonia: a Holistic Perspective. J Neural Transm (2021) 128(4):549–58. 10.1007/s00702-020-02265-0
47.
Bledsoe IO Viser AC San Luciano M . Treatment of Dystonia: Medications, Neurotoxins, Neuromodulation, and Rehabilitation. Neurotherapeutics (2020) 17(4):1622–44. 10.1007/s13311-020-00944-0
48.
Prudente CN Zetterberg L Bring A Bradnam L Kimberley TJ . Systematic Review of Rehabilitation in Focal Dystonias: Classification and Recommendations. Mov Disord Clin Pract (2018) 5(3):237–45. 10.1002/mdc3.12574
49.
De Pauw J Van der Velden K Meirte J Van Daele U Truijen S Cras P et al The Effectiveness of Physiotherapy for Cervical Dystonia: a Systematic Literature Review. J Neurol (2014) 261(10):1857–65. 10.1007/s00415-013-7220-8
50.
Wang W-L Chen K-H Pan Y-C Yang S-N Chan Y-Y . The Effect of Yoga on Sleep Quality and Insomnia in Women with Sleep Problems: a Systematic Review and Meta-Analysis. BMC Psychiatry (2020) 20(1):195. 10.1186/s12888-020-02566-4
51.
Gallagher A Kring D Whitley T . Effects of Yoga on Anxiety and Depression for High Risk Mothers on Hospital Bedrest. Complement Therapies Clin Pract (2020) 38:101079. 10.1016/j.ctcp.2019.101079
52.
Klingelhoefer L Kaiser M Sauerbier A Untucht R Wienecke M Mammadova K et al Emotional Well-Being and Pain Could Be a Greater Determinant of Quality of Life Compared to Motor Severity in Cervical Dystonia. J Neural Transm (2021) 128(3):305–14. 10.1007/s00702-020-02274-z
53.
Büssing A Ostermann T Lüdtke R Michalsen A . Effects of Yoga Interventions on Pain and Pain-Associated Disability: a Meta-Analysis. The J Pain (2012) 13(1):1–9. 10.1016/j.jpain.2011.10.001
Summary
Keywords
dystonia, complementary therapy, yoga, exercise, tele-rehabilitation
Citation
James-Palmer AM and Daneault J-F (2022) Tele-Yoga for the Management of Cervical Dystonia: A Safety and Feasibility Trial. Dystonia 1:10015. doi: 10.3389/dyst.2021.10015
Received
30 July 2021
Accepted
01 November 2021
Published
04 April 2022
Volume
1 - 2021
Edited by
Alfonso Fasano, Toronto Western Hospital, Canada
Reviewed by
Francesca Morgante, St George’s University Hospitals NHS Foundation Trust, London, United Kingdom
Ricardo Maciel, Universidade Federal de Minas Gerais, Brazil
Updates
Copyright
© 2022 James-Palmer and Daneault.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jean-Francois Daneault, jf.daneault@rutgers.edu
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.